Cornell University biomedical engineers have established a connection between the body’s normal inflammatory response and the way malignant breast cancer cells spread through the bloodstream, called metastasis. This finding suggests that treatment methods that focus on targeting the receptors and adhesion molecules on cancer cells may be able to reduce the spread of cancer cells and enhance current cancer treatments.
Biomedical engineers at Cornell University have discovered a link between the body’s natural inflammatory response and how malignant breast cancer cells use the bloodstream to metastasize, suggesting that therapeutic approaches targeting cytokine receptors and adhesion molecules on cancer cells may potentially reduce metastatic load and improve current cancer treatments.
Cancer is lethal because it spreads, or metastasizes, and curing cancer depends on knowing just how this process works. Cornell biomedical engineers have uncovered a groundbreaking link between the body’s natural inflammatory response, and how malignant breast cancer cells use the bloodstream to metastasize.
Their work, published online on January 23 in the open-access, peer-reviewed journal PLOS ONE, contends that pro-inflammatory signaling molecules in blood called cytokines constitute a “switch” that induces the mechanism by which breast cancer cells “roll” and adhere to the blood vessel surface. The cancer cells eventually stick to and infiltrate the vessel.
The paper’s first author is Yue Geng, graduate student in the field of biomedical engineering, working in the lab of Michael King, professor of biomedical engineering, who is the paper’s senior author.
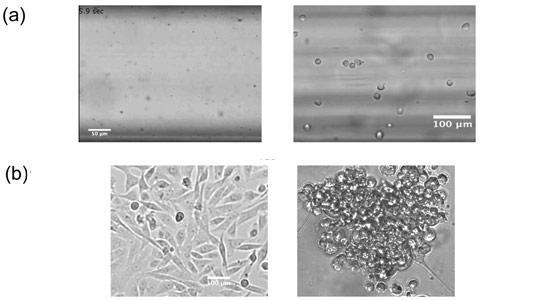
Image (a): Left: Untreated malignant breast cancer cells in a two-dimensional, standard culture medium show no interactions with selectin-coated surfaces under flow. Right: Cells establish stable rolling on selectin-coated surfaces after 48 hours of human plasma treatment.
Image (b): Left: Micrographs of breast cancer cells cultured in a standard two-dimensional monolayer. Right: a 3D tumor spheroid culture, which is physiologically closer to how cancer cells grow in the body. Credit: King Lab
King’s lab members study how cancer cells spread through the bloodstream by interacting with the blood vessel wall, called the endothelium. Cancer cells have small molecules, called ligands, on their surfaces that find specific receptor sites on the endothelium, called selectins. The ligand-selectin interaction causes the cells to literally “roll” on the endothelium, slowing down and eventually adhering to the blood vessel, in a process called the metastatic cascade. This mechanism is identical to how white blood cells infiltrate blood vessels to reach the site of inflammation.
Cancer has long been associated with inflammation — the body’s natural defense mechanism — and now the researchers have demonstrated a definitive link. They found that the presence of pro-inflammatory molecules — the cytokines IL-6 and TNF-alpha — enable the malignant, hormone therapy-resistant breast cancer cells used in the study to adhere to the endothelial wall, leading to metastasis.
Tumor cells first encounter IL-6 and TNF-alpha in the primary tumor’s microenvironment (before the cancer has spread). These cytokines induce proliferation and aggregation of cancer cells, triggering other cancer cells to secrete more cytokines, resulting in a positive feedback loop.
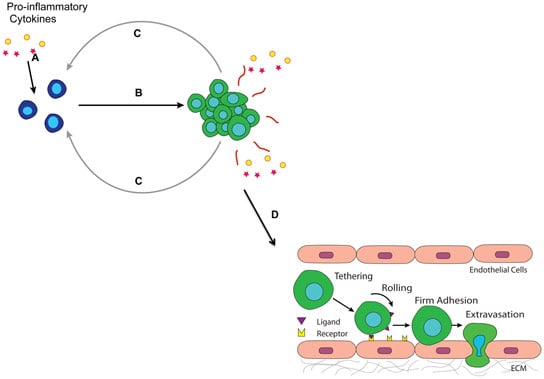
A positive feedback loop: activation and maintenance of the adhesive phenotypic switch. Step A: Tumor cells encounter proinflammatory cytokines such as IL-6 and TNF-α secreted by tumor-promoting immune cells in the microenvironment. Step B: Cytokine conditioned tumor cells form aggregates. Step C: Aggregates/spheroids of tumor cells release more IL-6 and TNF-α, turning on a phenotypic switch for more tumor cells nearby by upregulating E-selectin ligand and binding moiety expressions, and promote heterotypic interactions between tumor cells and the inflamed endothelium. Step D: Tumor cells ready to invade the endothelium. Credit: King lab
The King lab has developed a flow chamber that mimics inflamed endothelium and has used this to investigate the metastatic cascade on the bench top. In investigating the adhesive behavior of a particularly metastatic cell line, Geng and colleagues discovered unexpectedly that these cells were unable to interact with selectins — a key step in the metastatic cascade.
The bioengineers went on to design several different cell culture setups to culture cancer cells with human plasma, IL-6 and TNF-alpha to test their hypotheses that inflammatory molecules in blood may induce adhesion capability. All of them promoted breast cancer cell metastatic behavior.
They also used more sophisticated, 3D tumor spheroids, which are more physiologically accurate, to confirm their results. In fact, the 3D spheroid tumor cells exhibited the most significant increase in the interaction between the cancer cells and the blood vessel. They also treated some of the samples with a known anti-inflammatory drug called Metformin, which blocks IL-6, and they found that these samples were not able to metastasize — further underscoring their results.
Improving cancer treatment to fight metastasis via the bloodstream will depend on undoing this roll-and-stick mechanism of cancer cells, Geng said. The Cornell research could form the basis for immunotherapies to block the ligand-selectin binding of cancer cells, by first counteracting the inflammatory cytokines that, it seems, set the whole process in motion.
Reference: “Phenotypic Switch in Blood: Effects of Pro-Inflammatory Cytokines on Breast Cancer Cell Aggregation and Adhesion” by Yue Geng, Siddarth Chandrasekaran, Jong-Wei Hsu, Mishka Gidwani, Andrew D. Hughes and Michael R. King, 23 January 2013, PLOS ONE.
DOI: 10.1371/journal.pone.0054959
The research was funded by the National Cancer Institute via the Center on the Microenvironment and Metastasis, and a National Science Foundation Graduate Research Fellowship.








hope they will find out a cure for this bad dissea. Its worst one, and i think doctors need to work hard to have a solution about this