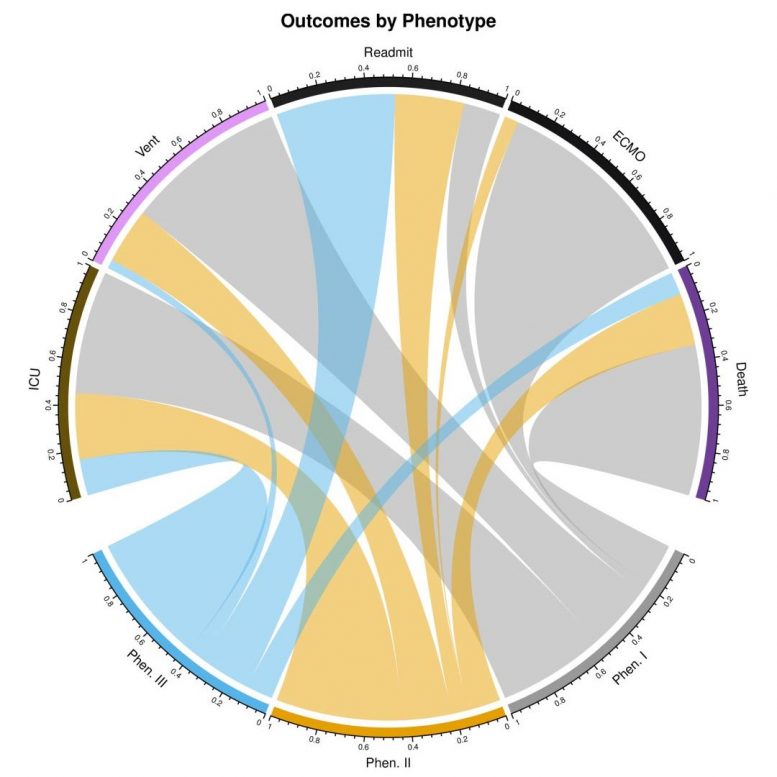
Clinical outcomes by phenotype. Chord diagram illustrates the prevalence of clinical outcomes (% observed) for the three clinical phenotypes. Abbreviations: ICU (intensive care unit); Vent (mechanical ventilation); Readmit (readmission to hospital or ICU); ECMO (extracorporeal membrane oxygenation). Credit: Lusczek et al, 2021, PLOS ONE (CC-BY 4.0)
Phenotypes I, II, and III show distinct characteristics and show adverse, normal, and favorable clinical outcomes respectively.
In a new study, researchers identify three clinical COVID-19 phenotypes, reflecting patient populations with different comorbidities, complications and clinical outcomes. The three phenotypes are described in a paper published this week in the open-access journal PLOS ONE 1st authors Elizabeth Lusczek and Nicholas Ingraham of University of Minnesota Medical School, US, and colleagues.
COVID-19 has infected more than 18 million people and led to more than 700,000 deaths around the world. Emergency department presentation varies widely, suggesting that distinct clinical phenotypes exist and, importantly, that these distinct phenotypic presentations may respond differently to treatment.
In the new study, researchers analyzed electronic health records (EHRs) from 14 hospitals in the midwestern United States and from 60 primary care clinics in the state of Minnesota. Data were available for 7,538 patients with PCR-confirmed COVID-19 between March 7 and August 25, 2020; 1,022 of these patients required hospital admission and were included in the study. Data on each patient included comorbidities, medications, lab values, clinic visits, hospital admission information, and patient demographics.
Most patients included in the study (613 patients, or 60 percent) presented with what the researchers dubbed “phenotype II.” 236 patients (23.1 percent) presented with “phenotype I,” or the “Adverse phenotype,” which was associated with the worst clinical outcomes; these patients had the highest level of hematologic, renal, and cardiac comorbidities (all p<0.001) and were more likely to be non-White and non-English speaking. 173 patients (16.9 percent) presented with “phenotype III,” or the “Favorable phenotype,” which was associated with the best clinical outcomes; surprisingly, despite having the lowest complication rate and mortality, patients in this group had the highest rate of respiratory comorbidities (p=0.002) as well as a 10 percent greater risk of hospital readmission compared to the other phenotypes. Overall, phenotypes I and II were associated with 7.30-fold (95% CI 3.11-17.17, p<0.001) and 2.57-fold (95% CI 1.10-6.00, p=0.03) increases in hazard of death relative to phenotype III.
The authors conclude that phenotype-specific medical care could improve COVID-19 outcomes, and suggest that future research is needed to determine the utility of these findings in clinical practice.
The authors add: “Patients do not suffer from COVID-19 in a uniform matter. By identifying similarly affected groups, we not only improve our understanding of the disease process, but this enables us to precisely target future interventions to the highest risk patients.”
Reference: “Characterizing COVID-19 clinical phenotypes and associated comorbidities and complication profiles” by Elizabeth R. Lusczek, Nicholas E. Ingraham, Basil S. Karam, Jennifer Proper, Lianne Siegel, Erika S. Helgeson, Sahar Lotfi-Emran, Emily J. Zolfaghari, Emma Jones, Michael G. Usher, Jeffrey G. Chipman, R. Adams Dudley, Bradley Benson, Genevieve B. Melton, Anthony Charles, Monica I. Lupei and Christopher J. Tignanelli, 31 March 2021, PLoS ONE.
DOI: 10.1371/journal.pone.0248956
Funding: 1. NIH National Heart, Lung, and Blood Institute T32HL07741 (NEI) 2. This research was supported by the Agency for Healthcare Research and Quality (AHRQ) and Patient-Centered Outcomes Research Institute (PCORI), grant K12HS026379 (CJT) and the National Institutes of Health’s National Center for Advancing Translational Sciences, grant UL1TR002494. 3. NIH National Heart, Lung, and Blood Institute T32HL129956 (JP, LS) The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.








Be the first to comment on "COVID-19 Patients Can Be Categorized Into Three Groups – Here Are the 3 Phenotypes"