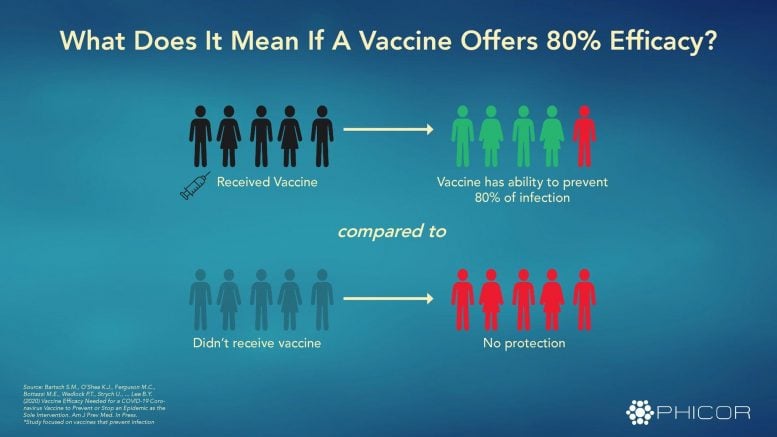
What does it mean if a COVID19 vaccine were to offer 80 percent efficacy? From “Vaccine Efficacy Needed for a COVID-19 Coronavirus Vaccine to Prevent or Stop an Epidemic as the Sole Intervention,” by Sarah M. Bartsch et al. https://doi.org/10.1016/j.amepre.2020.06.011 Credit: PHICOR
This question as well as coronavirus-related discrimination, population vulnerability, anxiety, and depression are explored in recent articles in the American Journal of Preventive Medicine
The American Journal of Preventive Medicine, published by Elsevier, is committed to publishing the most robust, evidence-based research and commentary on COVID-19 as they unfold to keep readers up to date and aware of issues relevant to community and individual health during this continually evolving global outbreak. All articles featured here are freely available.
New computational model finds that a COVID-19 vaccine will have to be at least 80 percent effective to achieve a complete “return to normal.”
Researchers around the world are racing to find a COVID-19 vaccine to eliminate the need for social distancing, mask-wearing, and limits on interpersonal gatherings. In a new study, a computer simulation model found that if 75 percent of the population gets vaccinated, the vaccine has to have an efficacy (ability to protect against infection) of at least 70 percent to prevent an epidemic and at least 80 percent to extinguish an ongoing epidemic.
If only 60 percent of the population gets vaccinated, the thresholds are even higher, around 80 percent to prevent an epidemic and 100 percent to extinguish an ongoing epidemic. “Some are pushing for a vaccine to come out as quickly as possible so that life can ‘return to normal.’
However, we have to set appropriate expectations. Just because a vaccine comes out doesn’t mean you can go back to life as it was before the pandemic,” notes lead investigator Bruce Y. Lee, MD, MBA, Public Health Informatics, Computational and Operations Research, CUNY Graduate School of Public Health and Health Policy, New York, NY, USA. “It is important to remember that a vaccine is like many other products — what matters is not just that a product is available, but also how effective it is.” The investigators say the results of their study can provide targets for vaccine developers as well as shape expectations for policy makers, business leaders, and the general public.
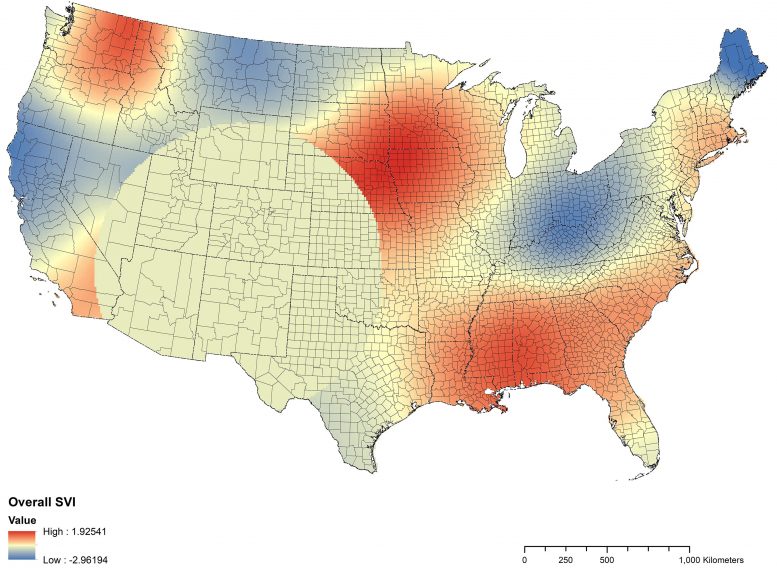
A coefficient map of social vulnerability to COVID-19 in the United States based on data collected through May 12, 2020. From “The Impact of Social Vulnerability on COVID-19 in the U.S.: An Analysis of Spatially Varying Relationships,” by Ibraheem M. Karaye, MD, DrPH, and Jennifer A. Horney, Ph.D., MPH. https://doi.org/10.1016/j.amepre.2020.06.006
Credit: American Journal of Preventive Medicine
“Vaccine Efficacy Needed for a COVID-19 Coronavirus Vaccine to Prevent or Stop an Epidemic as the Sole Intervention” by Sarah M. Bartsch, MPH, Kelly J. O’Shea, BSFS, Marie C. Ferguson, MSPH, Maria Elena Bottazzi, Ph.D., Patrick T. Wedlock, MSPH, Ulrich Strych, Ph.D., James A. McKinnell, MD, Sheryl S. Siegmund, MS, Sarah N. Cox, MSPH, Peter J. Hotez, MD, Ph.D., and Bruce Y. Lee, MD, MBA, 15 July 2020, American Journal of Preventive Medicine.
DOI: 10.1016/j.amepre.2020.06.011
Like indoor smoking bans, mask-wearing should be considered a fundamental occupational health protection.
Mask requirements to prevent the spread of COVID-19 are often presented as an infringement on individual rights. In this article, the authors note that bans against indoor smoking were enacted to protect workers’ health on the basis that individual rights do not extend to the imposition of risk on others. Similarly, masks should be required to protect workers by limiting the diffusion of particulates that carry COVID-19. Clear and consistent government policies on indoor mask-wearing would remove some of the burden from business owners, but in the absence of policy, business owners can also require masks, knowing that healthy workplaces have higher productivity. “Much like stepping outside to smoke, wearing a mask until the pandemic is resolved may feel like a nuisance; however both pose a relatively small inconvenience when compared to workers’ rights to a healthy, safe work environment,” observes lead author Mike Vuolo, PhD, Department of Sociology, The Ohio State University, Columbus, OH, USA.
“COVID-19 Mask Requirements as a Workers’ Rights Issue: Parallels to Smoking Bans” by Mike Vuolo, Ph.D., Brian C. Kelly, Ph.D., and Vincent Roscigno, Ph.D., 16 July 2020, American Journal of Preventive Medicine.
DOI: 10.1016/j.amepre.2020.07.001
Associations between social vulnerabilities and increased COVID-19 infection vary among US counties, suggesting need for different strategies to address the pandemic.
A new study confirms that social vulnerability is associated with increased prevalence of COVID-19 infection in the United States. However, the specific vulnerability factors most important in predicting infection — minority status and language, household composition and disability, and transportation and housing — vary among regions and counties. For example, in the Pacific Northwest, minority status and language and household composition and disability were more predictive of COVID-19 case counts. In the Gulf Coast states, housing and transportation were more predictive. Lead investigator Ibraheem M. Karaye, MD, DrPH, Epidemiology Program, University of Delaware, Newark, DE, USA, explains, “In the US, social vulnerability to COVID-19 is highly ‘local,’ so while a coordinated Federal response is needed to control COVID-19 nationally, local jurisdictions should, where possible given limited funding and staff, address specific vulnerable groups with interventions designed to mitigate the spread of the pandemic.”
“The Impact of Social Vulnerability on COVID-19 in the U.S.: An Analysis of Spatially Varying Relationships” by Ibraheem M. Karaye, MD, DrPH, and Jennifer A. Horney, PhD, MPH, 26 June 2020, American Journal of Preventive Medicine.
DOI: 10.1016/j.amepre.2020.06.006
Study identifies racial and socioeconomic disparities in testing and positive results for COVID-19 in New York City.
A new study has found that in New York City COVID-19 testing has not been proportional to need. Researchers conducted a statistical analysis on the relationship between race and socioeconomic factors such as household income, gross rent, poverty, education, working class status, and the rate of testing for the virus, and the proportion of positive results. They found that, adjusted for population, the total number of tests performed significantly increased in neighborhoods with more white residents, while the highest proportion of positive tests were recorded in nonwhite neighborhoods and in areas defined by lower socioeconomic status. “COVID-19 testing is a key component of public health efforts to contain the pandemic,” says lead investigator Emanuela Taioli, MD, PhD, Director, Institute for Translational Epidemiology;, Icahn School of Medicine at Mount Sinai; and Center for Disaster Health, Trauma, and Resilience, New York, NY, USA. “Our findings show that in New York City, there is an urgent need for widespread testing and public health outreach for the most vulnerable communities.”
“Disparities in COVID-19 Testing and Positivity in New York City” by Wil Lieberman-Cribbin, MPH, Stephanie Tuminello, MPH, Raja M. Flores, MD, and Emanuela Taioli, MD, PhD, 25 June 2020, American Journal of Preventive Medicine.
DOI: 10.1016/j.amepre.2020.06.005
Increase in mental distress during the rise of the COVID-19 pandemic associated with greater use of traditional and social media to learn about the disease.
In a nationally representative sample of US adults surveyed between March 10 and March 31, 2020, researchers found that individuals who reported spending more time on social media and consulting a greater number of traditional media sources to learn about the disease were more likely to report higher levels of mental distress than those with less media exposure. People who responded later in the survey, as a national emergency was declared and schools and businesses closed, reported greater media exposure and mental distress. “A pandemic of this scale in the era of social media is unprecedented. We need to consider how exposure to social media, and other sources of media like television or newspapers, might affect mental health during this time,” says first author Kira E. Riehm, MSc, Department of Mental Health, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, USA. The researchers suggest that engaging with supportive friends and family online and seeking information only from evidence-based sources like the CDC or WHO could support mental health.
“Associations Between Media Exposure and Mental Distress Among U.S. Adults at the Beginning of the COVID-19 Pandemic” by Kira E. Riehm, MSc, Calliope Holingue, PhD, Luther G. Kalb, PhD, Daniel Bennett, PhD, Arie Kapteyn, PhD, Qin Jiang, MA, Cindy Veldhuis, PhD, Renee M. Johnson, PhD, M. Daniele Fallin, PhD, Frauke Kreuter, PhD, Elizabeth A. Stuart, PhD, and Johannes Thrul, PhD, 10 July 2020, American Journal of Preventive Medicine.
DOI: 10.1016/j.amepre.2020.06.008
People thought to have COVID-19 can face discrimination, regardless of actual disease status, leading to increased anxiety and depression.
A national survey asked individuals if they were treated with less courtesy and respect than others; received poorer service at restaurants or stores; found people acted as if they were afraid of them; or felt threatened or harassed because they were suspected of having COVID-19. The rate of perceived discrimination, regardless of actual disease status, increased from March 2020, at the start of the pandemic, to April 2020. Asians and non-Hispanic blacks perceived more discrimination, as did individuals of any race or ethnicity who wore face masks. Perceiving discrimination was associated with increased anxiety and depression. Lead investigator Ying Liu, PhD, Center for Economic and Social Research, University of Southern California; Los Angeles, CA, USA, comments, “COVID-related discrimination is real and serious. It reflects social bias against racial and ethnic minorities and those who wear facemasks, and it disproportionately worsens mental despair in vulnerable populations. It is critical and timely for policy makers and the general public to become aware of this problem.”
“Perceived Discrimination and Mental Distress amid the 2019 Coronavirus Disease Pandemic: Evidence from the Understanding America Study” by Ying Liu, PhD, Brian Karl Finch, PhD, Savannah G. Brenneke, MPH, Kyla Thomas, PhD, and PhuongThao D. Le, PhD, MPH, 6 July 2020, American Journal of Preventive Medicine.
DOI: 10.1016/j.amepre.2020.06.007









Be the first to comment on "A COVID-19 Vaccine Doesn’t Need to Be Perfect to Stop the Pandemic – Here’s How Effective It Needs to Be"