Vaping-related lung injury and COVID-19’s shared symptoms can be confusing.
A UC Davis Health pediatric team presented a powerful case series of three teenagers who had unexplained breathing problems during the COVID-19 pandemic. The series highlighted the similarities between e-cigarette, or vaping, product use-associated lung injury (EVALI) and COVID-19 symptoms and manifestations.
“EVALI and COVID-19 share many symptoms but have very different treatment plans,” said Kiran Nandalike, associate professor of pediatrics and lead author on the study. “For this reason, providers caring for pediatric patients with unexplained respiratory failure should consider EVALI and ask for relevant smoking/vaping history.”
Teenagers facing COVID-19 and EVALI
As of February 2020, over 2758 EVALI hospitalized cases and 64 deaths have been reported in the U.S. More than half of those hospitalized were younger than 25 years old.
According to Nandalike, most adolescents who vape using recreational marijuana get the substance from friends, family members or unlicensed dealers. The unregulated access to these products is linked to continued outbreaks in this underage population. E-cigarette products obtained through these informal channels may contain vitamin E acetate, an additive strongly connected to lung injury.
Recent studies indicate that COVID-19-related practices may increase vaping among teenagers. Isolation from the school environment, loneliness, stress of the current pandemic, and lack of social support could increase the potential for substance use. This risk is especially true for young people with preexisting mental health conditions.
EVALI and COVID-19 common symptoms
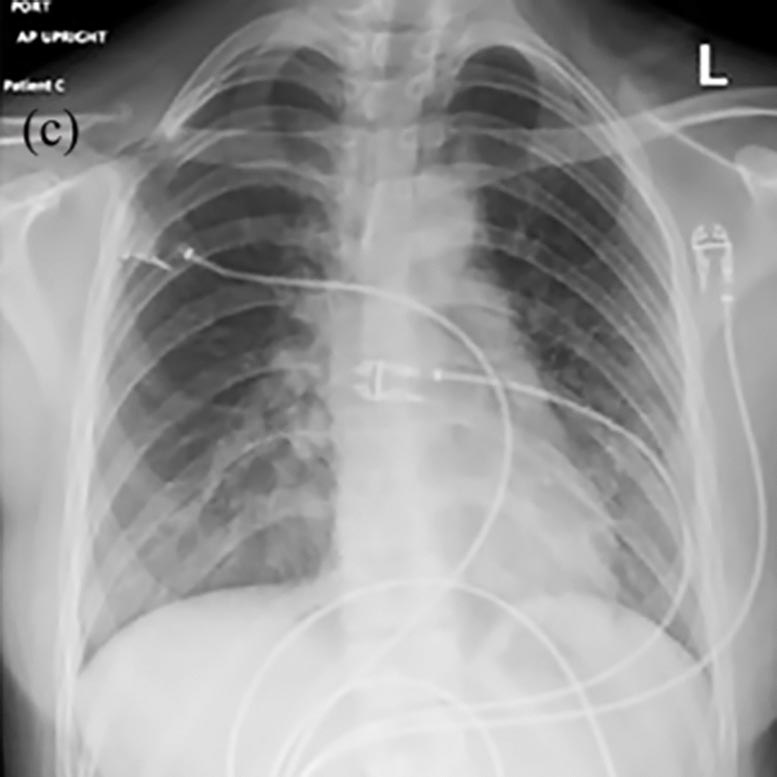
There are many similarities between EVALI and COVID-19 symptoms, laboratory results, and radiologic findings. Common symptoms include fever, cough, nausea, abdominal pain, and diarrhea. Both conditions also show bilateral ground glass opacities in chest imaging.
With the COVID-19 pandemic, it is easy to miss EVALI diagnosis. The patients in the case series showed up with fever, nausea, and cough. They had fast heart rate, rapid breathing and low oxygen levels in their blood. Their laboratory results pointed to inflammation commonly seen in COVID-19, with higher white blood cells (WBC) count and elevated inflammation. Their chest imaging revealed non-specific ground glass opacities. While everything indicated COVID-19 infection, their SARS-CoV-2 testing returned negative.
The providers probed the teenagers and their parents for any history of vaping in the last 90 days. When the patients shared information about recent vaping, the providers could diagnose EVALI and treat them successfully with corticosteroids.
Daphne Darmawan, pediatric resident at UC Davis Health and first author of the study, is looking at the clinical course and long-term health impacts of teenagers with EVALI. She is working on developing protocols to help with the early identification and treatment of these cases. Starting steroids early for patients with EVALI can be lifesaving and may minimize the duration of hospital stay.
“To help reduce the risk of EVALI recurrence, providers would recommend vaping cessation counseling to patients and close outpatient monitoring,” Nandalike said.
The article was published on October 30, 2020, in SAGE Open Medical Case Reports.
Reference: “Vaping in today’s pandemic: E-cigarette, or vaping, product use–associated lung injury mimicking COVID-19 in teenagers presenting with respiratory distress” by Daphne O Darmawan, Kriti Gwal, Brian D Goudy, Sanjay Jhawar and Kiran Nandalike, 30 October 2020, SAGE Open Medical Case Reports.
DOI: 10.1177/2050313X20969590
Co-authors on this study are Daphne O Darmawan, Kriti Gwal, Brian D. Goudy and Sanjay Jhawar at UC Davis Health.








Did not know you could vape pot. I thought you needed the product in a capsule to use the vape inhaler. Or perhaps marijuana comes in that form? It is amazing why we try to regulate bad things from happening to foolish people. They simply manage to change the route, the drug, the timing of damaging their brains first and then the rest of their bodies. Parents who leave access to these products or deliberately dose their children (see plenty of that in the ERs), do need prosecution. Let the rest of them do as they wish. I don’t wish to pay for their incarceration or supervision. Just remember, we don’t wish you driving, flying a plane, handling firearms, being a nurse, a doctor, etc. Drugs of all kinds limit your lifetime accomplishments in oh so many ways.
The lung injury isn’t caused by commercially available THC or nicotine based vaporizers. It’s coming from black market THC liquid. Drug dealers buy THC liquid from China and dilute it with vegetable oil to double their profit. It has a nearly identical color and viscosity so it’s impossible to detect. Unfortunately, these dealers didn’t realize that while the cooking oil vaporizes like the propylene glycol that’s supposed to be used in vape products, it condenses back into an oil as it cools in your lungs. That oily grease builds up in your lungs causing breathing problems and eventually an infection which has already killed dozens of people. Fortunately it seems like black market sellers began using propylene glycol since it’s just as cheap and it won’t kill anyone. Marijuana legalization is helping a lot. The states that prohibit marijuana use are seeing more cases of the lung injury. The only option for marijuana users in those states is to purchase black market products that aren’t regulated.