
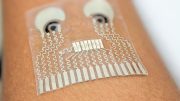
The device can be worn on the upper arm while the wearer goes about their day. Credit: Laboratory for Nanobioelectronics / UC San Diego
Imagine being able to measure your blood sugar levels, know if you’ve had too much alcohol to drink, and track your muscle fatigue during a workout, all in one small device worn on your skin. Engineers at the University of California San Diego (UCSD) have developed a prototype of such a wearable that can continuously monitor several health stats—glucose, alcohol, and lactate levels—simultaneously in real-time.
“This is like a complete lab on the skin.” — Joseph Wang
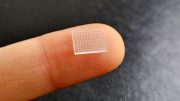
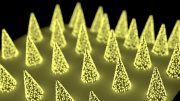
The multi-tasking device is only about the size of a stack of six quarters. It is applied to the skin through a Velcro-like patch of microscopic needles, or microneedles, that are each about one-fifth the width of a human hair. Wearing the device is not painful—the microneedles barely penetrate the surface of the skin to sense biomolecules in interstitial fluid, which is the fluid surrounding the cells beneath the skin. The device can be worn on the upper arm and sends data wirelessly to a custom smartphone app.
Researchers at the UC San Diego Center for Wearable Sensors describe their device in a paper published today (May 9, 2022) in the journal Nature Biomedical Engineering.
The device can be worn on the upper arm and sends data wirelessly to a custom smartphone app. Credit: Laboratory for Nanobioelectronics / UC San Diego
“This is like a complete lab on the skin,” said center director Joseph Wang, a professor of nanoengineering at UC San Diego and co-corresponding author of the paper. “It is capable of continuously measuring multiple biomarkers at the same time, allowing users to monitor their health and wellness as they perform their daily activities.”
Most commercial health monitors, such as continuous glucose monitors for patients with diabetes, only measure one signal. The problem with that, the researchers said, is that it leaves out information that could help people with diabetes, for example, manage their disease more effectively. Monitoring alcohol levels is useful because drinking alcohol can lower glucose levels. Knowing both levels can help people with diabetes prevent their blood sugar from dropping too low after having a drink. Combining information about lactate, which can be monitored during exercise as a biomarker for muscle fatigue, is also useful because physical activity influences the body’s ability to regulate glucose.
“With our wearable, people can see the interplay between their glucose spikes or dips with their diet, exercise, and drinking of alcoholic beverages. That could add to their quality of life as well,” said Farshad Tehrani, a nanoengineering Ph.D. student in Wang’s lab and one of the co-first authors of the study.
Microneedles merged with electronics
The wearable consists of a microneedle patch connected to a case of electronics. Different enzymes on the tips of the microneedles react with glucose, alcohol and lactate in interstitial fluid. These reactions generate small electric currents, which are analyzed by electronic sensors and communicated wirelessly to an app that the researchers developed. The results are displayed in real time on a smartphone.
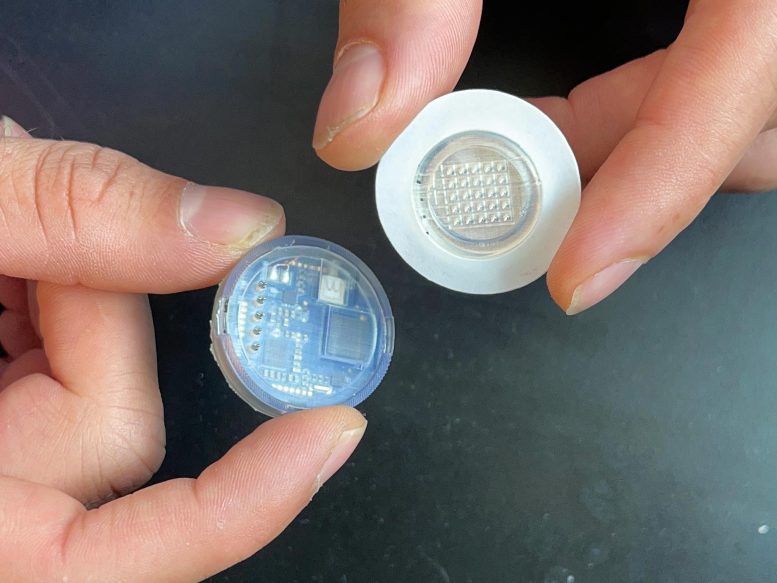
The disposable microneedle patch detaches from the reusable electronic case. Credit: Laboratory for Nanobioelectronics / UC San Diego
An advantage of using microneedles is that they directly sample the interstitial fluid, and research has shown that biochemical levels measured in that fluid correlate well with levels in blood.
“We’re starting at a really good place with this technology in terms of clinical validity and relevance,” said Patrick Mercier, a professor of electrical and computer engineering at UC San Diego and co-corresponding author of the paper. “That lowers the barriers to clinical translation.”
The microneedle patch, which is disposable, can be detached from the electronic case for easy replacement. The electronic case, which is reusable, houses the battery, electronic sensors, wireless transmitter, and other electronic components. The device can be recharged on any wireless charging pad used for phones and smartwatches.
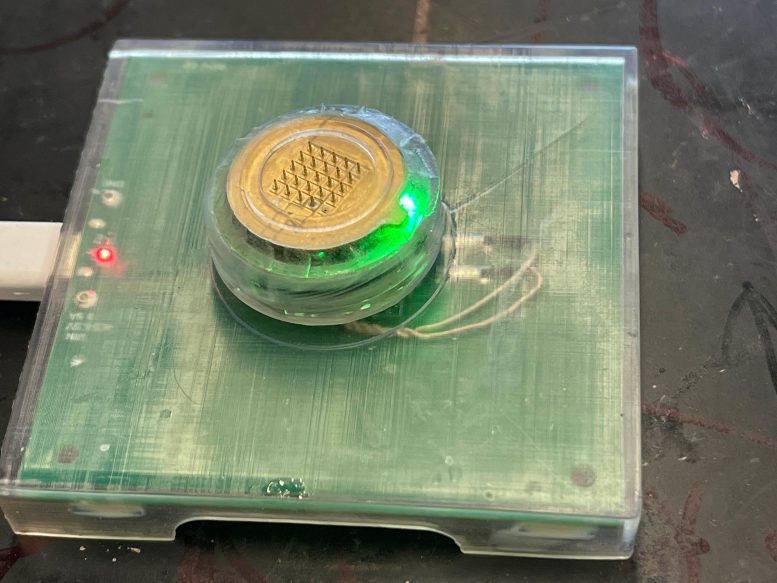
The device can be recharged on an off-the-shelf wireless charging pad. Credit: Laboratory for Nanobioelectronics / UC San Diego
Integrating all these components together into one small, wireless wearable was one of the team’s biggest challenges. It also required some clever design and engineering to combine the reusable electronics, which must stay dry, with the microneedle patch, which gets exposed to biological fluid.
“The beauty of this is that it is a fully integrated system that someone can wear without being tethered to benchtop equipment,” said Mercier, who is also the co-director of the UC San Diego Center for Wearable Sensors.
Testing
The wearable was tested on five volunteers, who wore the device on their upper arm, while exercising, eating a meal, and drinking a glass of wine. The device was used to continuously monitor the volunteers’ glucose levels simultaneously with either their alcohol or lactate levels. The glucose, alcohol and lactate measurements taken by the device closely matched the measurements taken respectively by a commercial blood glucose monitor, Breathalyzer, and blood lactate measurements performed in the lab.
Next steps
Farshad Tehrani and fellow co-first author Hazhir Teymourian, who is a former postdoctoral researcher in Wang’s lab, co-founded a startup company called AquilX to further develop the technology for commercialization. Next steps include testing and improving upon how long the microneedle patch can last before being replaced. The company is also excited about the possibility of adding more sensors to the device to monitor medication levels in patients and other health signals.
Reference: “An integrated wearable microneedle array for the continuous monitoring of multiple biomarkers in interstitial fluid” by Farshad Tehrani, Hazhir Teymourian, Brian Wuerstle, Jonathan Kavner, Ravi Patel, Allison Furmidge, Reza Aghavali, Hamed Hosseini-Toudeshki, Christopher Brown, Fangyu Zhang, Kuldeep Mahato, Zhengxing Li, Abbas Barfidokht, Lu Yin, Paul Warren, Nickey Huang, Zina Patel, Patrick P. Mercier and Joseph Wang, 9 May 2022, Nature Biomedical Engineering.
DOI: 10.1038/s41551-022-00887-1
Funding: NIH/National Institute of Neurological Disorders and Stroke






This would be perfect for measuring INR for blood thinners.
Technology such as this can really help when it come to living a normal life. As our technology advances so can our humanity, imagine how advanced our devices could be without profit margins. A device invented to do what it’s suppose to do without having to wait till a replicable part is invented for this already working device such as a cartridge order to keep you paying 2, 3 or 4 times a month for a device you fully paid for.
Six quarters thick? Good luck not knocking it off walking through doorways, etc….
Oh yes technology, cost not much for Big Pharm to make ,but what they charge a customer, well you have to have money. Cause if you don’t have the right insurance, an your deductible not met. They gave you a medical help cost to lower your costs for your 3 month,but my cost out of pocket every 3 months is almost $500.00 dollars every time I order a 3 months supply. Which on my budget. With my bills I pay,specialist doctors, an then com. I have a hard time coming up with that extra money. So I know why Type 1 Diabetic people have problems trying to live on products that cost way to much….When they should be cheaper so we Diabetic people can live longer.
I would like more information and contact with developers… this has huge clinical implications with disease management…. Can these devices be wireless, connected to EMR applications?, can they share safely over a network to accelerate care?