
Researchers have identified gut bacteria that are associated with dementia with Lewy bodies. Credit: Reiko Matsushita
Dementia with Lewy bodies (DLB) is a common form of dementia that currently has no cure. Previous research has suggested that the gut microbiome, or the microorganisms that reside in the human digestive tract, may play a role in the neurodegenerative disorder Parkinson’s disease. However, the specific bacteria involved in DLB have yet to be identified.
Now, a group led by researchers at the Nagoya University Graduate School of Medicine in Japan has identified three bacteria involved in DLB: Collinsella, Ruminococcus, and Bifidobacterium. Their findings, reported in the journal npj Parkinson’s Disease, suggest new avenues for diagnosis and treatment.
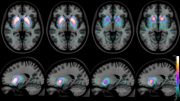
The onset of DLB is associated with abnormal deposits of alpha-synuclein, a protein in the brain that plays a role in the transmission of signals between neurons. The presence of these deposits, known as ‘Lewy bodies’, affects chemicals in the brain, leading to declines in thinking, reasoning, and memory. Symptoms include confusion, memory loss, impaired movement, and visual hallucinations.
Parkinson’s disease also starts with movement problems, but some patients develop cognitive decline within one year. These patients are diagnosed with DLB when this cognitive decline occurs. Physicians find it difficult to predict which people with Parkinson’s disease will develop cognitive decline within a year and become patients with DLB.
A research group led by Associate Professor Masaaki Hirayama (Omics Medicine), Professor Kinji Ohno (Neurogenetics), and Assistant Professor Hiroshi Nishiwaki (Neurogenetics) of Nagoya University Graduate School of Medicine, in collaboration with Okayama Neurology Clinic, Iwate Medical University, and Fukuoka University, analyzed microorganisms in the gut and fecal bile acids of patients with DLB, Parkinson’s disease, and rapid eye movement behavior disorder.
They discovered that three intestinal bacteria, Collinsella, Ruminococcus, and Bifidobacterium, were associated with patients with DLB. This may suggest possible ways of diagnosing and treating this neurodegenerative disease.
The researchers also found similarities between the gut bacteria involved in Parkinson’s disease and DLB. In both diseases, the bacteria Akkermansia, which degrades the intestinal mucosa, increased. On the other hand, the bacteria that produce short-chain fatty acids (SCFA) in the gut decreased. “Decreases in SCFA-producing bacteria have been repeatedly reported in Parkinson’s disease, Alzheimer’s disease, and ALS,” explains Ohno. “This suggests that it is a common feature of neurodegenerative diseases.” SCFA are important because they produce regulatory T cells. These types of cells play a critical role in regulating the immune system by suppressing neuroinflammation.
On the other hand, in patients with DLB, the researchers found an increase in Ruminococcus torques, an increase in Collinsella, and a decrease in Bifidobacterium. This was different from Parkinson’s disease patients, whose levels did not change. In the future using these insights, doctors may be able to analyze the bacteria in a person’s digestive tract to distinguish DLB from Parkinson’s disease.
Importantly, the reduced levels of Bifidobacterium may also suggest possible ways to treat DLB. Bifidobacterium increases brain-derived neurotrophic factor, a key protein that supports the growth, development, and maintenance of neurons in the central and peripheral nervous systems. Therefore, its decrease in DLB is likely to be associated with cognitive decline.
Similarly, both Ruminococcus torques and Collinsella are intestinal bacteria that carry an enzyme, the product of which regulates inflammation in a region of the brain called the substantia nigra. The substantia nigra produces dopamine, a neurotransmitter that is involved in the regulation of movement and is deficient in Parkinson’s disease. Compared to Parkinson’s disease, the levels of these bacteria were higher in people with DLB. This may explain why the effect on movement is delayed, a key feature that distinguishes DLB from Parkinson’s disease.
“Our findings can be used both for both diagnosis and treatment,” explains Ohno. “If a patient with Parkinson’s disease develops dementia in one year after the onset of motor symptoms, they are diagnosed with DLB. However, we cannot currently predict whether a patient with Parkinson’s disease will become a DLB patient. The gut microbiome will help to identify such patients.”
“In terms of treatment, the administration of Ruminococcus torques and Collinsella in patients with Parkinson’s is expected to delay neuroinflammation in the substantia nigra,” Ohno added. “Therapeutic intervention to increase Bifidobacterium may delay the onset and progression of DLB and reduce cognitive dysfunction.”
“The presence of intestinal bacteria unique to DLB may explain why some patients develop Parkinson’s disease and others develop DLB first,” Ohno said. “Normalizing the abnormal bacteria shared between DLB and Parkinson’s disease may delay the development of both diseases. Improving the gut microbiota is a stepping stone in the treatment of dementia. Our findings may pave the way for the discovery of new and completely different therapeutics.”
Reference: “Gut microbiota in dementia with Lewy bodies” by Hiroshi Nishiwaki, Jun Ueyama, Kenichi Kashihara, Mikako Ito, Tomonari Hamaguchi, Tetsuya Maeda, Yoshio Tsuboi, Masahisa Katsuno, Masaaki Hirayama and Kinji Ohno, 9 December 2022, npj Parkinson’s Disease.
DOI: 10.1038/s41531-022-00428-2








Always comes back to the gut biome – because current diets are far too heavy with packaged & processed foods that contain chemicals for the food’s appearance, flavor etc that may be destroying good gut bacteria. Taking a good supplement that contains those bacteria or even ACV with ‘mother’ puts all those good bacteria back where they belong. I got rid of my heart burn with daily ACV many years ago, and have always taken a multi-bug supp ever since ! No heartburn ever ! Let’s face it the food corporations do not care what those chemicals do to you as long as they sell the product !
This will be interesting info. For many people ,as since going through covid,I have been suffering many issues with my gut,heart and brain.
This is awesome news, as my husband passed with Lewy Bodies back in 2011. It is a terrible degenerative disease, and longevity is only really a few yrs. It had been misdiagnosed as Parkinson. I am glad this research has finally come to the forefront.