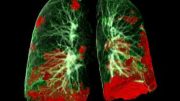
Scientists identified genes linked to antiviral immunity and lung inflammation provide key insights into COVID-19’s impact on lungs.
Potential treatments for COVID-19 have been identified after the discovery of five genes associated with the most severe form of the disease.
Genetic evidence is second only to clinical trials as a way to tell which treatments will be effective in a disease. Existing drugs that target the actions of the genes reveal which drugs should be repurposed to treat COVID-19 in clinical trials, experts say.
Genes involved in two molecular processes — antiviral immunity and lung inflammation — were pinpointed. The breakthrough will help doctors understand how COVID-19 damages lungs at a molecular level.
Researchers from the University of Edinburgh made the discovery by studying the DNA of 2,700 patients in 208 intensive care units (ICUs) in the UK.
Researchers from the GenOMICC consortium — a global collaboration to study genetics in critical illness — compared the genetic information of COVID-19 patients in ICU with samples provided by healthy volunteers from other studies, such as UK Biobank, Generation Scotland, and 100,000 Genomes.
The team found key differences in five genes of the ICU patients compared with samples provided by healthy volunteers. The genes — IFNAR2, TYK2, OAS1, DPP9, and CCR2 — partially explain why some people become desperately sick with Covid-19, while others are not affected.
Having highlighted the genes, the team were then able to predict the effect of drug treatments on patients, because some genetic variants respond in a similar way to particular drugs.
For example, they showed that a reduction in the activity of the TYK2 gene protects against Covid-19. A class of anti-inflammatory drugs called JAK inhibitors, which includes the drug baricitinib, produces this effect.
They also discovered that a boost in the activity of the gene INFAR2 is also likely to create protection, because it is likely to mimic the effect of treatment with interferon — proteins released by cells of the immune system to defend against viruses. However, experts caution that to be effective, patients might need the treatment early in disease.
Based on the findings published in Nature, the researchers say that clinical trials should focus on drugs that target these specific antiviral and anti-inflammatory pathways.
Dr. Kenneth Baillie, the project’s chief investigator and Academic Consultant in Critical Care Medicine and Senior Research Fellow at University of Edinburgh’s Roslin Institute, said: “This is a stunning realization of the promise of human genetics to help understand critical illness. Just like in sepsis and influenza, in Covid-19, damage to the lungs is caused by our own immune system, rather than the virus itself. Our genetic results provide a roadmap through the complexity of immune signals, showing the route to key drug targets.
“Our results immediately highlight which drugs should be at the top of the list for clinical testing. We can only test a few drugs at a time, so making the right choices will save thousands of lives.
“This work is only possible because of the generous contribution of the patients themselves and their families, research teams in NHS hospitals across the country, and the generous funding we’ve received from the public and organizations.”
GenOMICC (Genetics of Susceptibility and Mortality in Critical Care) started in 2015 as an open, global consortium of intensive care clinicians dedicated to understanding genetic factors that influence outcomes in intensive care from diseases such as SARS, influenza, and sepsis. Throughout 2020 it has been focused on COVID-19 research in partnership with Genomics England.
Reference: “Genetic mechanisms of critical illness in Covid-19” by Erola Pairo-Castineira, Sara Clohisey, Lucija Klaric, Andrew D. Bretherick, Konrad Rawlik, Dorota Pasko, Susan Walker, Nick Parkinson, Max Head Fourman, Clark D. Russell, James Furniss, Anne Richmond, Elvina Gountouna, Nicola Wrobel, David Harrison, Bo Wang, Yang Wu, Alison Meynert, Fiona Griffiths, Wilna Oosthuyzen, Athanasios Kousathanas, Loukas Moutsianas, Zhijian Yang, Ranran Zhai, Chenqing Zheng, Graeme Grimes, Rupert Beale, Jonathan Millar, Barbara Shih, Sean Keating, Marie Zechner, Chris Haley, David J. Porteous, Caroline Hayward, Jian Yang, Julian Knight, Charlotte Summers, Manu Shankar-Hari, Paul Klenerman, Lance Turtle, Antonia Ho, Shona C. Moore, Charles Hinds, Peter Horby, Alistair Nichol, David Maslove, Lowell Ling, Danny McAuley, Hugh Montgomery, Timothy Walsh, Alex Pereira, Alessandra Renieri, The GenOMICC Investigators, The ISARICC Investigators, The COVID-19 Human Genetics Initiative, 23andMe Investigators, BRACOVID Investigators, Gen-COVID Investigators, Xia Shen, Chris P. Ponting, Angie Fawkes, Albert Tenesa, Mark Caulfield, Richard Scott, Kathy Rowan, Lee Murphy, Peter J. M. Openshaw, Malcolm G. Semple, Andrew Law, Veronique Vitart, James F. Wilson and J. Kenneth Baillie, 11 December 2020, Nature.
DOI: 10.1038/s41586-020-03065-y
This study is one of a number of COVID-19 studies that have been given urgent public health research status by the Chief Medical Officer and Deputy Chief Medical Officer for England.
GenOMICC is funded by the charity Sepsis Research FEAT, the Intensive Care Society, Wellcome, UK Research and Innovation, Scotland’s Chief Scientist Office, and the Department of Health and Social Care via the National Institute for Health Research.







Perhaps this also explains how many early news stories focused on entire families being wiped out that were in contact with each other, while others were relatively untouched since many genes tend to be passed on, particularly if the genes aren’t recessive?
Notably, the HIV virus also has a type of gene link in that people without the key blood cell receptors generally speaking cannot contract at least one version of AIDS from it as it has nowhere to attach. Notably significant parts of Western Europe have natural immunity due to the infamous Black Plague of the Middle Ages apparently coincidentally used the same receptor and killed most of the population that had the receptor, leaving large populations of descendants with the gene for the missing receptor in those regions. I believe many of the drugs that keep AIDS at bay fill that receptor with a harmless molecule, preventing large scale infection of the blood cells with HIV and this was due to the (accidental?) discovery of a researcher testing remains from the infamous plague.
Thus, it may be possible that certain regions have greater or lesser populations with resistant genes, which may explain why countries like Norway and Finland have had such low death rates despite mostly not wearing masks and minimal lockdowns compared to parts of Europe more heavily hit despite the more strict measures. Perhaps even in parts of Asia it’s not all due to contact tracing and masking. They may have more people with similar genes that just happen to be beneficial at not getting as ill with the Coronavirus? Alternatively, they may have had exposure to similar protein structure common cold viruses that trigger an immune response to Covid, providing chance (at least partial) immunity. Several hypothesis have been proposed over the year. More than one may play a part in explaining why some regions are seemingly hit harder than others despite employing similar measures of lockdowns, contact tracing, social distancing and masking.