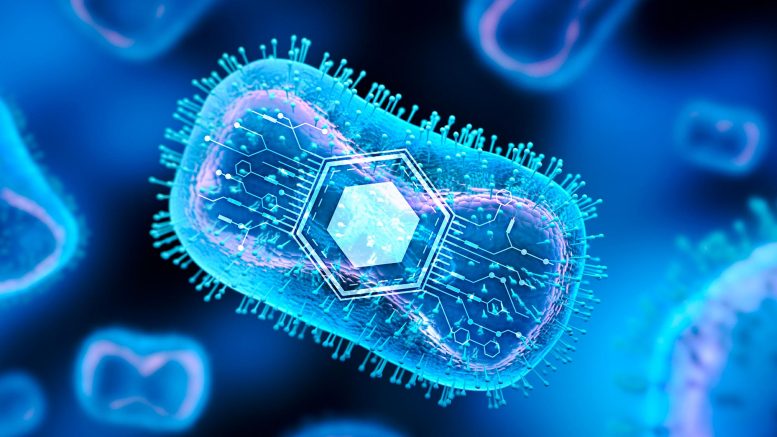
Investigators are developing synthetic programmable bacteria to help kill cancerous tissue. Credit: Texas A&M Engineering
Texas A&M University researchers are co-leading a $20 million project to develop a $1 cancer treatment.
What if a single one-dollar dose could cure cancer?
A multi-university team of researchers, supported by federal funding, is developing a highly efficient bacterial therapeutic to target cancer more precisely to make treatment safer through a single $1 dose.
Traditionally, cancer therapies have been limited in their efficacy in treating patients. Some, like radiation and chemotherapy, cause harmful side effects, while others tend to result in low patient responsiveness, not to mention the cost it takes to receive treatment. Findings from the American Cancer Society Cancer Action Network recorded that 73% of cancer survivors and patients were worried about how they were going to pay the cost of their cancer care, and 51% said they were in medical debt from treatment. For example, state-of-the-art cancer therapy can cost up to $1,000,000.
Texas A&M University and the University of Missouri are leading the effort to develop a low-cost, safe, and controlled cancer treatment. Researchers received a $20 million grant from the Advanced Research Projects Agency for Health (ARPA-H) to fight cancer. The four-year project is part of the current administration’s Cancer Moonshot initiative, an effort to advance and increase funding for cancer research. It is one of the first projects funded by the newly established agency that aims to accelerate better health outcomes for everyone by supporting the development of high-impact solutions to society’s most challenging health problems.
Rapidly Analyzing Cells
$12 million of the grant will go to the Texas A&M Engineering Experiment Station/Texas A&M, where co-principal investigators Drs. Arum Han, Jim Song and Chelsea Hu are developing synthetic programmable bacteria for immune-directed killing in tumor environments (SPIKEs). The idea is to engineer bacteria to help T cells kill cancerous tissue, destroy itself once the cancer is gone, and leave the body safely as human waste.
“SPIKEs can specifically target tumor cells,” said Han, the Texas Instruments Professor in the Department of Electrical and Computer Engineering. “And since it’s only targeting cancerous tissue and not the surrounding healthy cells, the safety of the patient is exponentially increased. It’s a great honor to be on this team, tackling a major health problem that affects a lot of people.”
Han’s lab is developing high-throughput microfluidic systems that can rapidly process and screen massive bacterial therapeutic libraries, one cell at a time, to quickly identify the most promising treatments. These systems are enabled by integrating microfabrication methods and biotechnology to achieve a pico-liter-volume liquid handling system that can accurately analyze single cells with high precision and high speeds, creating devices to analyze individual cells quickly.
“The major challenge is figuring out how to actually develop these sophisticated microdevices that allow us to conduct millions and millions of fully automated tests with almost no manual or human intervention,” Han said. “That’s the engineering challenge.”
Rescuing Anti-Tumor Immune Cells
While Han innovates and designs microdevices, Song — an immunologist with a background in microbial pathogenesis, T cell biology and T cell-based immunotherapy — has been working on bacteria immunotherapy for the past five years. A certain bacteria known as Brucella Melitensis can manipulate the microenvironment of the human body and promote T cell-mediated anti-tumor immunity to treat at least four types of cancers.
“We are working to improve Brucella Melitensis to more efficiently prevent or suppress tumor growth,” said Song, a professor at the Texas A&M School of Medicine. “Our current approach involves finding out how to engineer bacteria to rescue anti-tumor immune cells, enhancing their effectiveness in killing tumor cells.
“Data so far shows that Brucella’s efficiency is dramatically higher than other cancer treatments, such as Chimeric antigen receptor T cell therapy and T-cell receptor therapies, with a more than 70% responsiveness rate,” Song said.
Safe And Controllable Therapeutics
While Song continues to test the bacteria’s efficiency using cancer models, Hu, an assistant professor in the Artie McFerrin Department of Chemical Engineering and a synthetic biologist, is working to ensure the living bacterial therapeutic is safe and controllable.
“The Brucella strain we’re using has been shown to be safe for the hosts because it is an attenuated version, meaning a key gene that is required for bacteria virulence has been deleted,” Hu said. “Ultimately, we want to control the bacterium’s rate of growth, where it grows within the tumor environment, and its ability to self-destruct when its mission is completed.”
To control the growth rate, the bacterium’s genes will be altered to regulate its population and oscillate around a specific setpoint. Hu also plans to engineer biosensors into the bacteria, enabling them to differentiate between healthy tissue and tumor tissues to ensure they grow only within the tumor microenvironment.
The bacterium will be engineered to have a receptor to ensure that once the cancer is gone, the patient can take antibiotics that will signal the bacterium to essentially cut itself into pieces and be removed safely from the patient’s body.
“As humans, we’re actually covered in bacteria, and a lot of diseases are caused by an imbalance in these bacterial communities,” Hu said. “For instance, while some people have incredibly fragile stomachs, others have robust ones. The science behind it is that those people with strong immune and digestive systems have a healthy community of bacterial cells in their gut. There’s a lot of potential in living therapeutics.”
“It’s a really great opportunity to have an incredible team who have expertise and can push this technology to the front line,” Hu said. “So that sort of goal is to reach the clinic and provide patients with an effective cancer treatment at less than $1 per dose.”
Attacking Difficult Issues Using Unconventional Approaches
Other collaborators include Dr. Zhilei Chen at the Texas A&M Health Science Center and Dr. Xiaoning Qian in the Department of Electrical and Computer Engineering, along with the principal investigator, Dr. Paul de Figueiredo, from Missouri University.
“The three key advantages to this work are high safety, low cost, and specific targeting of cancerous tumors,” Han said. “We are very excited that we are one of the first teams that are getting support from ARPA-H, which is a brand-new agency established and supported by Congress to really tackle hard problems in broad areas of health. We’re attacking difficult issues using unconventional approaches. High risk, high impact is the hallmark of our approach.”
And the future applications of engineering bacteria that this research unlocks are limitless.
“For our next big project, we will work together to engineer bacteria against autoimmune diseases such as type 1 diabetes and rheumatoid arthritis,” Song said. Bacterium-based immunotherapy represents a groundbreaking frontier in medicine, offering the potential to revolutionize the treatment of autoimmune diseases. With the power of beneficial microbes harnessed to modulate the immune system, we are on the verge of changing the future of medicine. Our research and expertise hold the promise of transforming the lives of millions of people, providing them with new hope and healthier tomorrows.”







Be the first to comment on "The $1 Cure: How Programmable Bacteria Are Reshaping Cancer Therapy"