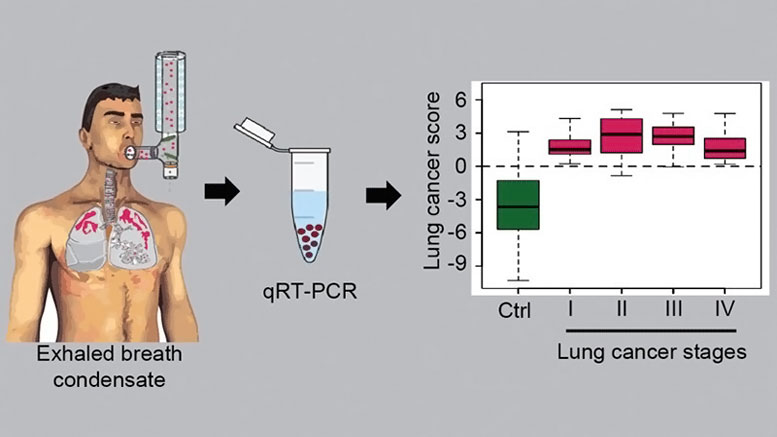
Researchers can collect RNA molecules released from lung tissue and amplify them with the help of polymerase chain reaction (qRT-PCR). The molecules can serve as a diagnostic tool to detect cancer cells in the lungs.
Researchers at the Max Planck Institute have developed a method that can detect the disease at an early stage. New research on healthy volunteers and cancer patients shows that the breath test correctly determined the health status of 98 percent of the participants. The method will now be refined in cooperation with licensing partners so that it can be used for the diagnosis of lung cancer.
Most lung cancer patients die within five years of diagnosis. One of the main reasons for this is the insidious and largely symptom-free onset of the disease, which often remains unnoticed. In the USA, high-risk groups, such as heavy smokers, are therefore routinely examined by CAT scan. However, patients can be wrongly classified as having the disease.
Together with cooperation partners, scientists at the Max Planck Institute for Heart and Lung Research have now developed a breath test that is much more accurate. In their research, the diagnosis of lung cancer was correct in nine out of ten cases. The method is therefore reliable enough to be used for the routine early detection of lung cancer.
The scientists analyzed RNA molecules released from lung tissue into expired breath, noting differences between healthy subjects and lung cancer patients. Unlike DNA, the RNA profile is not identical in every cell. Several RNA variants, and therefore different proteins, can arise from one and the same DNA segment. In healthy cells, such variants are present in a characteristic ratio. The scientists discovered that cancerous and healthy cells contain different amounts of RNA variants of the GATA6 and NKX2 genes. Cancer cells resemble lung cells in the embryonic stage.
The team developed a method to isolate RNA molecules. Not only is their concentration in expired breath extremely low, but they are also frequently highly fragmented. The scientists then investigated the RNA profile in subjects with and without lung cancer and from these data established a model for diagnosing the disease. In a test of 138 subjects whose health status was known, the test was able to identify 98 percent of the patients with lung cancer. 90 percent of the detected abnormalities were in fact cancerous.
“The breath test could make the detection of early-stage lung cancer easier and more reliable, but it will not completely supplant conventional techniques,” says Guillermo Barreto, a Working Group Leader at the Max Planck Institute in Bad Nauheim. “However, it can complement other techniques for detecting early cancer stages and reduce false-positive diagnoses.”
The researchers will contribute to future large-scale clinical trials. Together with the technology transfer organization Max Planck Innovation, they are seeking licensing partners to develop the breath test to maturity and market it. They also hope to use RNA profiles for the early detection of other diseases. Tiny changes could produce tissue profiles, akin to an RNA fingerprint, that reveal diseased cells and allow for rapid treatment.
Reference: “Non‐invasive lung cancer diagnosis by detection of GATA6 and NKX2‐1 isoforms in exhaled breath condensate” by Aditi Mehta, Julio Cordero, Stephanie Dobersch, Addi J Romero-Olmedo, Rajkumar Savai, Johannes Bodner, Cho-Ming Chao, Ludger Fink, Ernesto Guzmán-Díaz, Indrabahadur Singh, Gergana Dobreva, Ulf R Rapp, Stefan Günther, Olga N Ilinskaya, Saverio Bellusci, Reinhard H Dammann, Thomas Braun, Werner Seeger, Stefan Gattenlöhner, Achim Tresch, Andreas Günther and Guillermo Barreto, 7 November 2016, EMBO Molecular Medicine.
DOI: 10.15252/emmm.201606382







when was this invented or studied. I need that info for a school project.
Publication: Aditi Mehta, et al., “Non‐invasive lung cancer diagnosis by detection of GATA6 and NKX2‐1 isoforms in exhaled breath condensate,” EMBO Molecular Medicine (2016) 8, 1380-1389; DOI 10.15252/emmm.201606382