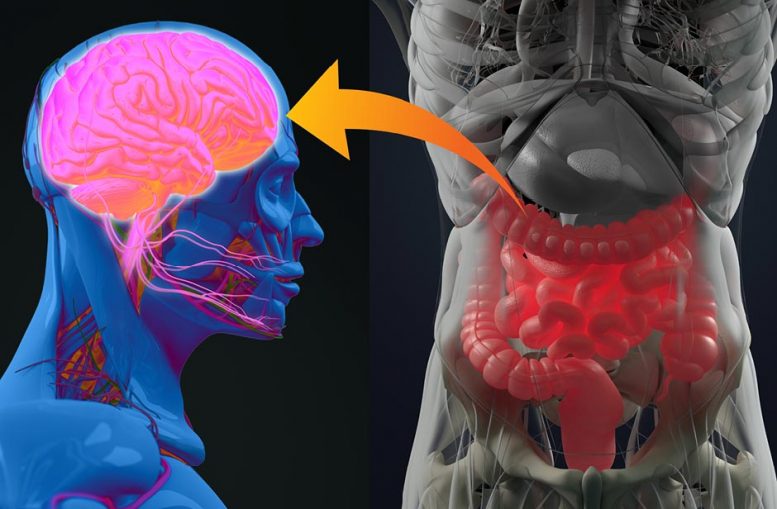
Patrice Cani (UCLouvain) and Claude Knauf (INSERM) have discovered a ‘jammer’ that blocks communication between the gut and the brain, thus preventing proper regulation of sugar and causing insulin resistance in people with diabetes. They also discovered that a lipid produced by our body helps prevent this dysfunction and regulate sugar level, thus mitigating diabetes and intestinal inflammation. These discoveries, published in the scientific journal GUT, are major, because today one in two Europeans is overweight and one in ten has diabetes. Credit: UCLouvain
Since 2004, Claude Knauf (INSERM) and Patrice Cani (Université Catholique de Louvain) have been collaborating on molecular and cellular mechanisms in order to understand the causes of the development of type 2 diabetes and above all to identify new therapeutic targets. In 2013, they created an international laboratory, ‘NeuroMicrobiota Lab’ (INSERM-UCLouvain), to identify links between the brain and intestinal bacteria.
Very quickly, they understood that the gut-brain axis plays a preponderant role in the regulation of sugar in the blood. When we eat, the gut (also called the ‘second brain’ owing to the neurons that compose it) contracts and digests food. Sugar and fat enter the body and their levels increase in the blood. Using this sugar and fat, the body then does its work or stores them. In a person with diabetes, this process malfunctions and the sugar level increases in abnormal proportions.
Taking a step further, the two researchers observed that the gut, when it digests, sends a signal to the brain, to find out what to do with the incoming fats and sugars. The brain then sends the message to various organs (liver, muscles, adipose tissue) to get ready to lower blood sugar and fat levels. In a diabetic individual, however, this mechanism doesn’t work. Researchers have observed that the gut malfunctions and sends no signal to the brain. The cause is hypercontractility of the intestine, which interferes with communication with the brain. Suddenly, commands to get the sugar out of the blood no longer pass. The sugar remains, causing hyperglycaemia. The mechanism also impacts the action of insulin: no message means no insulin action, resulting in insulin resistance.
The researchers sought to understand this hypercontractility, by observing the differences in the constitution of the intestine as well as the action of prebiotics within the microbiota in ‘normal’ and ‘diabetic’ mice. They observed that a particular lipid was severely deficient in diabetic mice, but also in people with diabetes (although it’s naturally present in the intestines of healthy patients). The team therefore tested the impact of the lipid on the use of sugars, on the contraction of the intestine and, ultimately, on diabetes. NeuroMicrobiota research team members Anne Abot and Eve Wemelle discovered the lipid is the key to restoring the use of sugar. It works by acting directly on the second brain.
Today, the team has discovered and understood how our gut bacteria (or gut microbiota) play an important role in altering the production of bioactive lipids, and from there to restore perfect communication between the gut and the brain. Hence some of these lipids are essential messengers that act on very precise targets in the second brain (enkephalins or opioid receptors). Treatment possibilities include modifying the body’s production of such lipids, could or taking them orally. These avenues are under study.
Using the same approach, the INSERM-UCLouvain research team, contributed to the discovery of a new bioactive lipid that reduces intestinal inflammation. It is directly produced by certain gut bacteria, also identified in this study and therefore the two approaches, either the lipid or one or more bacteria, could serve as a therapeutic target.
One in three of the 150,000 humans who die every day is a victim of cardiovascular disease, according to WHO. Half the Belgian population is overweight and presents cardiovascular and type 2 diabetes risks. This UCLouvain and INSERM research could potentially have an impact on a large portion of the population.
Reference: “Identification of new enterosynes using prebiotics: roles of bioactive lipids and mu-opioid receptor signalling in humans and mice” by Anne Abot, Eve Wemelle, Claire Laurens, Adrien Paquot, Nicolas Pomie, Deborah Carper, Arnaud Bessac, Xavier Mas Orea, Christophe Fremez, Maxime Fontanie, Alexandre Lucas, Jean Lesage, Amandine Everard, Etienne Meunier, Gilles Dietrich, Giulio G Muccioli, Cedric Moro, Patrice D Cani and Claude Knauf, 5 October 2020, Gut.
DOI:
To carry out this research, UCLouvain’s Patrice Cani received funding from several sources including WELBIO, FNRS and the Baillet-Latour Fund.







Very Interesting.
There was a Japanese Post Doctrol student working on making a Cyclopropyl tri -peptide on a sugar tripppeptide” to create sweeter version of Saccharine used currently across the globe.
He was successful in converting the double bond to a cyclopropyl tri-peptide. It was sent to a lab to test for its sweeetness. If I remember correctly , it was found to be about 60 tmes sweeter.However, it was also found to be addictive, so I dont think it was every released to the public at large. This was around 1977 to 1980.
There was also a loy of other very interesting research going on inluding modifications on enkaphlins which are the active component of “Happy” in endorphins. Thi was also from 1980.
It may be smart to capture all such scientific research in digital mode and make it acessible to the Scientific Community globally, especially in light of the Opiod Crisis being faced by many nations. Also, no point in reinventing the wheel. All progress is built on the newer generation standing on the shoulders of gaints who have come before us.
This may become evenmore critical as in the eternal battle between the huuman immunity ecosystem defense and bacteria, pathogens and viruses, the re-emergence of the superbugs and future pandemics like SUPER Scarleet fever , where it appears that bacteria ad virus are co-operating to infect Children is extremely worrying. We will need to shore up the knowledge base and also improve the Human Ecosystem Immunity and shore it up, and also avoid introducing foods into the human ecosystem which compromises the same and allows such disease causing entities to enter and create havoc.