
The study revealed that individuals with cardiovascular disease might face a twofold increase in COVID-19 fatality risk. Moreover, various pre-existing conditions could elevate the risk of death by one-and-a-half to three times in COVID-19 patients.
A large, international study of COVID-19 patients confirmed that cardiovascular disease, hypertension, diabetes, congestive heart failure, chronic kidney disease, stroke, and cancer can increase a patient’s risk of dying from the virus. Penn State College of Medicine researchers say their findings may help public health officials improve patient care and develop interventions that can target these high-risk populations.
The researchers found that cardiovascular disease may double a patient’s risk of dying from COVID-19. They also discovered that other pre-existing conditions may increase a COVID-19 patient’s risk of death by one-and-a-half to three times. The results were recently published in PLOS ONE.
“This study suggests that these chronic conditions are not just common in patients with COVID-19, but their presence is a warning sign to a higher risk of death,” said Dr. Paddy Ssentongo, a doctoral student in epidemiology at the College of Medicine and research assistant professor in Penn State’s Department of Engineering Science and Mechanics. “There is a high prevalence of cardiovascular disease and hypertension around the world and in particular, the U.S. With the persistence of COVID-19 in the U.S., this connection becomes crucially important.”
The research team conducted a systematic review and meta-analysis of studies published from December 2019 through early July 2020, to determine which chronic conditions put hospitalized patients at risk of dying from COVID-19. They explored 11 co-existing conditions that pose a risk of severe disease and death among COVID-19 patients, including cardiovascular disease, diabetes, high blood pressure, cancer, chronic kidney disease, chronic obstructive pulmonary disease, stroke, congestive heart failure, asthma, chronic liver disease, and HIV/AIDS.
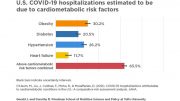
Ssentongo and colleagues analyzed data from more than 65,000 patients from 25 studies worldwide. Patients in the selected studies had an average age of 61 years. They found that certain pre-existing health conditions affected survival rates more than others. When compared to hospitalized COVID-19 patients without pre-existing conditions, researchers determined that patients with diabetes and cancer are 1.5 times more likely to die, patients with cardiovascular disease, hypertension, and congestive heart failure are twice as likely to die, and patients with chronic kidney disease are three times more likely to die.
“Although the health care community has circulated anecdotal information about the impact of these risk factors in COVID-19 mortality, our systematic review and meta-analysis is the most comprehensive to date that attempts to quantify the risk,” said Vernon Chinchilli, distinguished professor and chair of public health sciences, and senior author of this research. “As the COVID-19 pandemic continues through 2020 and likely into 2021, we expect that other researchers will build on our work.”
The researchers said that prior studies exploring the association of pre-existing chronic conditions and COVID-19 mortality had limitations in the number of countries included, the number of studies included and the number of conditions explored. They also said these studies had unaddressed sources of bias that limited the conclusions that can be drawn from them.
“We took an all-inclusive, global approach for this study by examining 11 chronic conditions and including patients from four continents: Asia, Europe, North America and Africa,” Ssentongo adds. “Research suggests that SARS-CoV-2, the virus that causes COVID-19, may become seasonal and require annual vaccination. Once an approved and effective vaccine is available, high-risk individuals with these pre-existing conditions should receive vaccination priority to prevent high mortality rates.”
Even though additional research is needed to fully understand health risks and implications, particularly in understanding the effects of race and ethnicity on COVID-19 survival rates, Ssentongo said these findings can help inform global prevention and treatment strategies.
Reference: “Association of cardiovascular disease and 10 other pre-existing comorbidities with COVID-19 mortality: A systematic review and meta-analysis” by Paddy Ssentongo, Anna E. Ssentongo, Emily S. Heilbrunn, Djibril M. Ba and Vernon M. Chinchilli, 26 August 2020, PLOS ONE.
DOI: 10.1371/journal.pone.0238215
Djibril Ba, Emily Heilbrunn and Anna Ssentongo from Penn State College of Medicine also contributed to this research.
The researchers received no specific funding for this study and declare no conflicts of interest.








REBEL’S DAILY REPORTS
Read facebook.com/ron.mccune.3 for more info about the coronavirus and ways to easily stop the spread of the coronavirus. Here now I will explain to you my observations about how the virus works inside the body and how to maybe help cure those that get it.
The coronavirus shows to be a certain type of virus that has a life span inside of a body. The way it behaves inside a body depends first on how much of the virus actually enters your body. If a lot of coronavirus molecules enter your body then you will have a harder time fighting off the coronavirus than those that have a lot less coronavirus molecules entering the body. The coronavirus has only three ways to enter your body, either through your mouth, nose, or eyes. The amount of coronavirus entering your body is important because the coronavirus first has a life span inside one’s body. You catch the virus, you get sick and die or recover. Some people do have longer lasting illnesses but the majority of people infected with the coronavirus go through the whole process from infected to recovery in about 2-3 weeks for mild cases and up to 3 months for serious cases. So there seems to be something going on here with this coronavirus where some get it worse than others. With knowledge known now why that is so it is important to look at what we are doing to make it so. The thing I noticed is that many of those that got seriously ill or died from coronavirus were I believe, from my observation, people who did a lot of mingling with other people and mingled longer and also mingled closely, a foot or less in distance with people, which also helped them to get more of the virus in them than say someone who got a certain low amount of the virus from a brief encounter with an infected individual from more than a foot away. So the amount of virus you get in you seems to say how much you will get sick and how. So it would then seem very logical that we all practice safe guidelines to insure that we don’t get any coronavirus in us. We should all wear facemask that are capable of stopping the spread of the coronavirus. Wearing a facemask that doesn’t for sure stop the coronavirus from infecting you or you infecting others is a irresponsible and possibly deadly decision to make! Protect yourselves and others is the only way we are going to slow or stop this coronavirus epidemic! We all have to chip in and do our part to initiate a mandatory time right now to wear a facemask before it’s too cold or snowy or windy or difficult to wear facemask! We all should participate in a nation wide mandatory safe practicing mode from 1-2 months to stop the increase of people getting the coronavirus. Then after the 1-2 month mandatory safe practice time we can see how many are still catching the coronavirus. When one is then identified as being sick with the coronavirus they will then be isolate, no charge, in special coronavirus care facilities that are to be for coronavirus infected people only. Coronavirus infected people will be isolated from the general public until they are cured. No more putting those with coronavirus in hospitals and nursing homes or their own homes to fight the coronavirus where they could then infect others which is what is going on with the spread of this coronavirus. That is how China help stop the coronavirus a lot in their crowded country and that is what we have to do here in America to really slow down the infection rate of coronavirus.
But getting back to what I believe is what happens when the coronavirus enters the body. The coronavirus illness may be able to be better controlled or managed if maybe we were to do all we can to flush out the digestive system once one becomes ill from coronavirus. Maybe flushing out the digestive system would also flush out whatever coronavirus molecules are lingering in the digestive system. Also try giving coronavirus patients lots of water to help flush out their bladder and to dilute their bodies fluids. Then try giving coronavirus patients a healthy protein rich food as often as possible throughout the day. Also give them 2 extra strength multi vitamins/minerals a day 6-8 hours apart with a protein rich meal that contains all the 9 amino acids that the human body needs to make a perfect cell of any kind. I recommend a recipe called Adelynn’s Miracle Beans recipe which has all the 9 proteins in abundance that the body needs to make any kind of body cell. Just maybe by giving the body food and vitamins that has all the 9 amino acids, vitamins and minerals that are needed to make any kind of human cell then that super duper glob of biological wonder we call our brain will figure out ways to use the proteins and vitamins to create new cells to fight off the coronavirus! Why not try it? What have you got to lose? You already are losing lives so why not try this way I suggest to try to help people with the coronavirus. More on my facebook page. More to be posted in the future about this and other subjects on my facebook page.