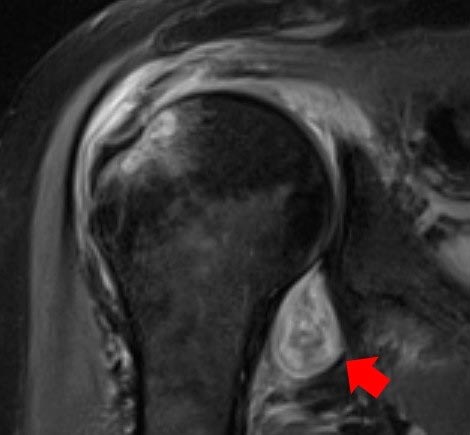
MRI image of a patient’s shoulder. The red arrow points to inflammation in the joint. The COVID virus triggered rheumatoid arthritis in this patient with prolonged shoulder pain after other covid symptoms resolved. Credit: Northwestern University
Imaging illustrates severity, long-term prognosis of COVID-19-related muscle, joint pain.
Muscle soreness and achy joints are common symptoms among COVID-19 patients. But for some people, symptoms are more severe, long-lasting, and even bizarre, including rheumatoid arthritis flares, autoimmune myositis or “COVID toes.”
A new Northwestern Medicine study has, for the first time, confirmed and illustrated the causes of these symptoms through radiological imaging.
“We’ve realized that the COVID virus can trigger the body to attack itself in different ways, which may lead to rheumatological issues that require lifelong management,” said corresponding author Dr. Swati Deshmukh.
The paper will be published today (February 17, 2021) in the journal Skeletal Radiology. The study is a retrospective review of data from patients who presented to Northwestern Memorial Hospital between May 2020 and December 2020.
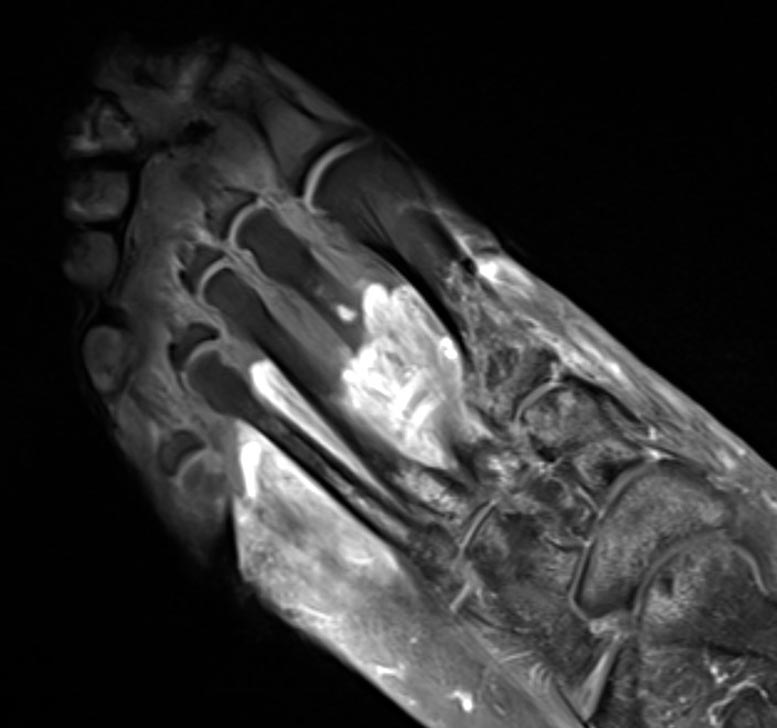
MRI of the foot in a patient with severe COVID-19. The grey part of the foot is devitalized tissue (gangrene). Credit: Northwestern University
“Many patients with COVID-related musculoskeletal disorders recover, but for some individuals, their symptoms become serious, are deeply concerning to the patient or impact their quality of life, which leads them to seek medical attention and imaging,” said Deshmukh, an assistant professor of musculoskeletal radiology at Northwestern University Feinberg School of Medicine and a Northwestern Medicine musculoskeletal radiologist. “That imaging allows us to see if COVID-related muscle and joint pain, for example, are not just body aches similar to what we see from the flu — but something more insidious.”
Imaging (CT, MRI, ultrasound) can help explain why someone might have prolonged musculoskeletal symptoms after COVID, directing them to seek the right physician for treatment, such as a rheumatologist or dermatologist.
In some cases, radiologists may even suggest a COVID diagnosis based on musculoskeletal imaging in patients who previously didn’t know they contracted the virus, Deshmukh said.
What does the imaging look like?
“We might see edema and inflammatory changes of the tissues (fluid, swelling), hematomas (collections of blood) or devitalized tissue (gangrene),” Deshmukh said. “In some patients, the nerves are injured (bright, enlarged) and in others, the problem is impaired blood flow (clots).”
How can imaging lead to better treatment?
“I think it’s important to differentiate between what the virus causes directly and what it triggers the body to do,” Deshmukh said. “It’s important for doctors to know what’s happening in order to treat correctly.”
For example, Deshmukh said, if a patient has persistent shoulder pain that started after contracting COVID, their primary care provider might order an MRI/ultrasound. If a radiologist knows COVID can trigger inflammatory arthritis and imaging shows joint inflammation, then they can send a patient to a rheumatologist for evaluation.
“Some doctors request imaging for patients with ‘COVID toes,’ for example, but there wasn’t any literature on imaging of foot and soft tissue complications of COVID,” Deshmukh said. “How do you find something if you’re unsure of what to look for? So in our paper, we discuss the various types of musculoskeletal abnormalities that radiologists should look for and provide imaging examples.”
Reference: “Musculoskeletal involvement of COVID-19: review of imaging” by Santhoshini Leela Ramani, Jonathan Samet, Colin K. Franz, Christine Hsieh, Cuong V. Nguyen, Craig Horbinski and Swati Deshmukh, 18 February 2021, Skeletal Radiology.
DOI: 10.1007/s00256-021-03734-7
Other Northwestern authors on the paper were Santhoshini Leela Ramani (Northwestern University medical student), Dr. Jonathan Samet (radiology), Dr. Colin Franz (PMR and neurology), Dr. Christine Hsieh (rheumatology), Dr Cuong Nguyen (dermatology) and Dr. Craig Horbinski (pathology).








I have had both shoulders and hands aching so bad since Covid a year ago only to be treated with multiple steroid shots , still have the pain leaving me with less things I can do , due to inability to perform because of weakness and severe pain