
Researchers have uncovered a devastating health crisis requiring urgent action: less than 7 percent of the U.S. adult population has good cardiometabolic health.
Researchers at Tufts University found that most U.S. adults rate poorly across five components of heart and metabolic health, with clear racial disparities.
Scientists have uncovered a devastating health crisis requiring urgent action: less than 7% of the U.S. adult population has good cardiometabolic health. This is according to a study led by a team from the Friedman School of Nutrition Science and Policy at Tufts University in a pioneering perspective on cardiometabolic health trends and disparities that will be published in the July 12 issue of the Journal of the American College of Cardiology. Their research team also included scientists from Tufts Medical Center.
“These numbers are striking. It’s deeply problematic that in the United States, one of the wealthiest nations in the world, fewer than 1 in 15 adults have optimal cardiometabolic health.” — Meghan O’Hearn
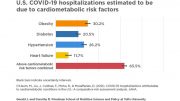
In the study, researchers evaluated Americans across five components of health: levels of blood pressure, blood cholesterol, blood sugar, adiposity (overweight and obesity), and presence or absence of cardiovascular disease (heart attack, stroke, etc.) They discovered that only 6.8% of U.S. adults had optimal levels of all five components as of 2017-2018. Among these five components, trends between 1999 and 2018 also worsened significantly for blood glucose and adiposity. In 1999, 1 out of 3 adults had optimal levels for adiposity (no overweight or obesity), but by 2018, that number decreased to 1 out of 4. Similarly, while 60% of adults didn’t have diabetes or prediabetes in 1999, fewer than 40% of adults were free of these conditions in 2018.
“These numbers are striking. It’s deeply problematic that in the United States, one of the wealthiest nations in the world, fewer than 1 in 15 adults have optimal cardiometabolic health,” said Meghan O’Hearn, a doctoral candidate at the Friedman School and the study’s lead author. “We need a complete overhaul of our healthcare system, food system, and built environment, because this is a crisis for everyone, not just one segment of the population.”
The study looked at a nationally representative sample of about 55,000 people aged 20 years or older from 1999 to 2018 from the 10 most recent cycles of the National Health and Nutrition Examination Survey. The researchers focused on optimal, intermediate, and poor levels of cardiometabolic health and its components, rather than just presence or absence of disease. “We need to shift the conversation, because disease is not the only problem,” O’Hearn said. “We don’t just want to be free of disease. We want to achieve optimal health and well-being.”
The team also identified large health disparities between people of different sexes, ages, races and ethnicities, and education levels. For example, adults with less education were half as likely to have optimal cardiometabolic health compared with adults with more education, and Mexican Americans had one-third the optimal levels versus non-Hispanic White adults. Additionally, between 1999 and 2018, while the percentage of adults with good cardiometabolic health modestly increased among non-Hispanic White Americans, it went down for Mexican American, other Hispanic, non-Hispanic Black, and adults of other races.
“We don’t just want to be free of disease. We want to achieve optimal health and well-being.” — Meghan O’Hearn
“This is really problematic. Social determinants of health such as food and nutrition security, social and community context, economic stability, and structural racism put individuals of different education levels, races, and ethnicities at an increased risk of health issues,” said Dariush Mozaffarian, dean of the Friedman School and senior author. “This highlights the other important work going on across the Friedman School and Tufts University to better understand and address the underlying causes of poor nutrition and health disparities in the U.S. and around the world.”
The study also assessed “intermediate” levels of health—not optimal but not yet poor—including conditions like pre-diabetes, pre-hypertension, and overweight. “A large portion of the population is at a critical inflection point,” O’Hearn said. “Identifying these individuals and addressing their health conditions and lifestyle early is critical to reducing growing healthcare burdens and health inequities.”
The consequences of the dire state of health among U.S. adults reach beyond personal health. “Its impacts on national healthcare spending and the financial health of the entire economy are enormous,” O’Hearn said. “And these conditions are largely preventable. We have the public health and clinical interventions and policies to be able to address these problems.”
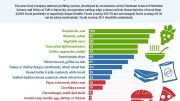
Researchers at the Friedman School work actively on many such solutions, O’Hearn said, including Food is Medicine interventions (using good nutrition to help prevent and treat illness); incentives and subsidies to make healthy food more affordable; consumer education on a healthy diet; and private sector engagement to drive a healthier and more equitable food system. “There are a lot of different avenues through which this can be done,” O’Hearn said. “We need a multi-sectoral approach, and we need the political will and desire to do it.”
“This is a health crisis we’ve been facing for a while,” O’Hearn said. “Now there’s a growing economic, social and ethical imperative to give this problem significantly more attention than it has been getting.”
Reference: “Trends and Disparities in Cardiometabolic Health Among U.S. Adults, 1999-2018” by Meghan O’Hearn MS, Brianna N. Lauren MS, John B.Wong MD, David D. Kim PhD and Dariush MozaffarianMD, DrPH, 4 July 2022, Journal of the American College of Cardiology.
DOI: 10.1016/j.jacc.2022.04.046
Funding: NIH/National Heart, Lung and Blood Institute







Although you make much mention of food in this article, you only hinted at the other major factor: Lack of exercise. The built environment in the U.S. is almost entirely centered on the private motor vehicle as the default means for transportation. This results in suburban and ex-urban sprawl that feeds on itself, with the result that these days, hour-long, 40-mile commutes each way to and from work are almost normal. The heavy expense of driving a car into the ground every few years increases pressure to work longer hours in locations that are often further away than would otherwise be necessary. After ten hours in the office plus two hours commuting, not many have time or energy left to cook a decent meal or get any exercise–especially if the exercise can only be had safely by spending even more time on the road to and from the gym.
If our built environment were set up so that cycling were a more practical and accepted way of getting around, at least the exercise component would take care of itself. Moreover, when a person gets enough exercise, they tend to crave foods that are better for them than when they don’t. Not many people feel like trying to fuel an hour a day on the bike with junk food. Currently, “America Runs on Dunkin”, and therein lies the problem.
Unfortunately, after spending nearly a century unquestioningly adopting the car-based lifestyle and building our infrastructure around the requirements of cars, we’re pretty much stuck with what we’ve got. I see little chance of effective leadership in the U.S. to get people to crawl out of their cars and adopt a more healthful lifestyle any time soon.
In 1980 the US FDA approved the expanded use of added ‘cultured free’ MSG. The US obesity/diabetes epidemic presented by 1990 (CDC/NCHS data). The rest is just history of ignorant and incompetent medical professionals before and since, as I only gradually and intermittently discovered since 1990 and recently formulated in some detail.
Approximate etiology and pathology of most chronic disease (T = time): subclinical non-IgE-mediated allergy reactions + offending foods + T + MSG/soy (minimally; less T) > inflammation + T > xanthine oxidase + T > serum uric acid (gout) + ROS (free radicals) + T > immunodeficiency + T > calcium (minimally) loss + T > acidic blood + T > mitochondria switching from glycolysis (glucose-to-energy) to glycogenesis (glucose-to-fat) + T > uric acid deactivating nitric oxide + T > oxidative stress + T > insulin resistance + T > metabolic syndrome (e.g. chronic fatigue, aches, pains, muscle weakness and brain fog) + T > chronic/degenerative disease (e.g. aging, Alzheimer’s, ALS, AMD, anxiety, bad moods [confusion; depression; mass shootings; suicides], cancer, cataracts, CFS/ME & FM, diabetes, gout, HBP, insomnia, obesity, stroke, tinnitus, tooth loss, etc.) and/or medical error + T > premature disability and/or death.
Our future adults who are now children need more nutritious school breakfasts and lunches. I have witnessed children partaking of a sugary cereal with chocolate milk for breakfast. Why not some oatmeal and fruit? No wonder these children have a hard time focusing and sitting still in the classroom! These children are in the process of establishing habits which will carry over into adulthood. We can do better!
Susan, as I try to explain in some detail above, it is not “we” who need to do better it is the people we pay to ‘protect and serve” us who need to do better. I was something of a ‘sugar-freak’ as a child and it never hurt me like FDA approved MSG has. Anecdotally, fructose, even as real fruit juice and as opposed to dextrose and glucose, can raise one’s uric acid unregulated.
Sugar is killing our livers and that is where the heart disease ends up coming from, i.e. when all your mitochondria become enzymatically dysfunctional, then comes the insulin resistance, industrial food might not shortern your life, but it is clearly causing many to start dying younger and younger. We are clearly not as smart as advertised, we seem quite dumb, weak, and self-destructive actually, particularly in how we’ve ruined food for profit. Oh wait, we are doing that to the entire planet now too, sigh.
M Brian, please don’t blame me for yours or anyone else’s insulin resistance and/or fatty liver disease. I’ve been trying to get that 1980 FDA approval of the expanded use of added ‘cultured free’ MSG reversed for sixteen years and counting. The ‘dumb, weak and self-destructive’ ones are the politicians and public officials of both major parties who accept bribes as campaign contributions (minimally) from the rich and the rich corporations; an illness industry evolved into a national healthcare crisis and now a ‘silent American genocide.’