As the Delta variant spreads, COVID-19 vaccines remain crucial to protecting children, elderly people and immunocompromised individuals. “We can’t care about just ourselves anymore,” said Prof. Kathleen Mullane. “We have to care about all of humanity.”
University of Chicago Prof. Kathleen Mullane discusses COVID-19 variants, and why vaccines are still so important.
The Delta variant of SARS-CoV-2, the virus that causes COVID-19, has already spread to more than 100 countries. As a result, we’re seeing more children being infected and hospitalized with the Delta variant compared to original strains of the virus.
“I am particularly concerned about the populations of people, including children, who have no immunity to COVID-19 because they have not yet been vaccinated,” said Prof. Kathleen Mullane, an infectious diseases expert at UChicago Medicine.
In the Q&A below, Mullane provides answers to common questions about variants—including an explanation of how viruses mutate, and why widespread vaccination remains our best defense against COVID-19.
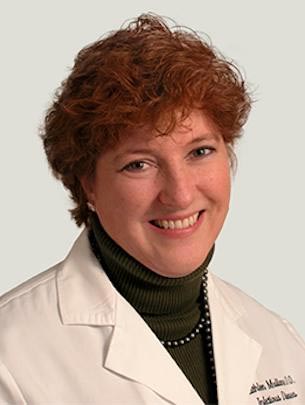
Prof. Kathleen Mullane
What is a variant, and where do variants come from?
A variant is a group of viruses that share an inherited set of distinctive mutations in their genetic code.
RNA viruses mutate; it’s what they do. When a virus replicates or makes copies of itself, errors can occur in the instructions (the RNA template) as they’re being read. In other words, the virus has a misprint. All coronaviruses have an enzyme called an error-correcting polymerase, which removes that incorrect insertion (misprint) in the RNA and replaces it with a “better one.” The better one, however, is not always perfect.
Sometimes, the mutation can be terminal, meaning the virus can’t replicate anymore and dies off. Other times, there’s no significant change in the virulence of the virus and its characteristics remain unchanged. Sometimes, however, the mutation causes a significant change in the genome, making a virus more transmissible and infectious.
How quickly does a virus mutate?
Some viruses, like influenza, can mutate quickly, while others change more slowly. SARS-CoV-2 mutates two to six times more slowly than influenza. What has made SARS-CoV-2 so troublesome is that the general population hasn’t had immunity to this coronavirus sub-genus. That means many more people are being infected with it than we would see with influenza, which is a virus we all have some baseline immunity to due to past infections or immunizations.
The more people are infected with a virus, the more it circulates, which causes more infections. As more people are infected, there’s a greater chance it mutates and leads to the circulation of multiple strains. As more strains circulate, there is a greater chance for recombination between strains. That’s when new variants occur.
We don’t know whether these variants are going to be more or less aggressive in the future, but we are very concerned we could see the development of viruses that are more aggressive and that our vaccines ultimately may not be able to protect us.
How do the Delta variant and potential other variants affect vaccinated vs. unvaccinated people?
Unvaccinated people are at high risk of becoming ill with the Delta variant. When we look at hospitalizations right now, between 90% and 97% of people who are in the hospital have the SARS-CoV-2 Delta variant and are unvaccinated.
For those who are vaccinated, a Delta variant infection generally feels like a mild upper respiratory illness with a cough, headache, sore throat and some muscle aches that are short lasting. Very few people end up losing their sense of smell or taste. One unusual finding that we’ve seen is there are more people complaining of ear pain, which is different from the initial coronavirus infection. Most importantly, very few vaccinated people are hospitalized and even fewer patients die from infection with the Delta variant.
“Unvaccinated people are at high risk of becoming ill with the Delta variant. … Very few vaccinated people are hospitalized and even fewer patients die from infection.”
— Prof. Kathleen Mullane
How are the variants affecting pregnant people?
Even before the Delta variant appeared, the mortality in pregnant people was found to be three times higher than in non-pregnant individuals—they’re a very vulnerable population. Delta is too new to be able to have data specifically regarding pregnant people, but we know it is more transmissible and is at least as pathogenic as the other SARS-CoV-2 variants that we’ve already experienced.
Many more people are getting infected with the Delta variant, which means more virus is in the community. That puts pregnant people at a much higher infection risk.
We are also now seeing babies infected, too. Infants don’t develop an immune system until they’re about 6 months old. We know a vaccinated person who gives birth passes some immune protection to their baby, which is another reason vaccination is so important, especially among those who are pregnant.
Are the current COVID-19 vaccines effective against variants?
The efficacy of our current vaccines is variable. The messenger RNA (mRNA) and the Johnson & Johnson/Janssen vaccines appear to be effective against hospitalizations and deaths due to infection with the existing variants. The Sinovac vaccine and some other adenovirus-based vaccines produced outside the U.S. don’t appear to be as effective as the mRNA vaccines. Worldwide, physician-scientists are looking at giving patients who were vaccinated with Sinovac or those other vaccines a dose of mRNA vaccine to see if that enhances their immunity.
Currently, our vaccines are effective against variants. We can look at efficacy of the mRNA vaccines in two studies that have been published: one in the United Kingdom and one in Israel. In the study done in the U.K., they showed 88% efficacy against symptomatic disease after two doses of an mRNA vaccine and 33% after a single dose. However, when they looked at hospitalizations, they reported 96% vaccine efficacy against hospitalization after two doses and 94% after one dose.
In Israel, the results were different. In early June, before Delta really became the predominant circulating SARS-CoV-2 variant, they reported about a 64% vaccine efficacy in preventing infection, or symptomatic disease. However, by the end of June and the beginning of July, the vaccine was only 39% effective against the Delta strain. When they looked at serious illness, the vaccine was 93% effective against serious illness or hospitalization, and by the end of July vaccine efficacy was 91% against serious illness and had fallen to 88% against hospitalization.

Although vaccinated people have tested positive for COVID-19 as a result of breakthrough infections, these individuals are far less likely to be at risk for serious illness from the Delta variant. Credit: Jakayla Toney
The AstraZeneca vaccine was reported to have 60% vaccine efficacy against symptomatic disease after two doses but only 33% after one dose. However, vaccine efficacy was 93% against hospitalizations, which is the important variable — meaning people are not getting seriously ill with COVID-19. For Johnson & Johnson, there was still good vaccine efficacy: 79% against symptomatic disease after two doses and 96% against hospitalization after two doses.
In the U.S., we had an experiment in situ, one might say. Barnstable County in Massachusetts saw an uptick in cases after multiple summertime parties when public health officials traced 469 COVID-19 cases back to these gatherings. However, we don’t know the total number of people involved in these events. Of those 469 people, 347 were fully vaccinated, which meant they either had two doses of mRNA or had a single shot of the Johnson & Johnson vaccine. Of those 347 vaccinated individuals, 274 were symptomatic. That left 75 people who tested positive for SARS-CoV-2 having no symptoms of infection at all.
The common symptoms reported in the 347 symptomatic patients were cough, headache, sore throat, muscle pain, and fever. Overall, five of the 469 people who tested positive were hospitalized with COVID-19. Four of those five were fully vaccinated. This means that only 1% of those vaccinated patients who developed COVID-19 were hospitalized. There were no deaths reported. They did strain testing on those who tested positive and of the 133 specimens that were sequenced, 90% were Delta variant.
This outbreak investigation led to the new recommendations for reinstituting universal masking because the Delta variant has now become the predominant circulating SARS-CoV-2 in the United States.
How dangerous is a variant?
That depends on the variant. In the case of the Delta variant, it is the most transmissible variant to date. The World Health Organization is calling it a “faster and fitter” virus.
Some people think it’s the most spreadable or transmissible virus that has ever occurred. With the original Wuhan strain, one person on average infected two to three others. With the Delta variant, one person infects five to eight people. This exponential spread has made it the most dominant of the SARS-CoV-2 coronavirus variants. It spreads 50% faster than the Alpha variant (the variant that arose in the United Kingdom), and Alpha was 50% faster than the Wuhan variant. This makes the Delta variant of SARS-CoV-2 a super-spreader.
If people aren’t vaccinated and are not masked, the spread of the Delta variant is very similar to the spread that we would see with chickenpox (varicella-zoster virus). When I was a kid, parents would have “chickenpox parties” to make sure that every kid in the neighborhood got it at the same time, and the infection would run through the neighborhood all at once instead of in dribs and drabs.
The varicella virus is so contagious that a non-immune person just being in the same room with an infected individual had a 99% chance of becoming infected with the virus and coming down with chickenpox. In the case of smallpox, we see between three and four people being infected from someone who has active smallpox if they are not protected by vaccination.
“The most important way future variants can be prevented is to develop herd immunity through mass vaccination.”
— Prof. Kathleen Mullane
How do we stop future variants from forming?
The most important way future variants can be prevented is to develop herd immunity through mass vaccination. We need to get the amount of circulating virus down, and to do this at least 80% of the entire population needs to be vaccinated. The more people who are vaccinated, the fewer people are going to be ill, which lessens the risk of the virus spreading and mutating. When people carry the virus, we get multiple strains of the virus, and that’s when we’re going to see a higher likelihood for a resistant variant to arise.
The other things we need to keep doing are masking, social distancing, and washing our hands. Especially in crowded areas, we want people to wear masks. We want people to social distance, especially if they’re indoors. Finally, we need to prevent super-spreader events where people are unvaccinated by mandating proof of vaccination in events where crowds may occur.
Again, vaccination is the single most important thing we can do.
What do we know about the Lambda and Gamma variants?
We already know Lambda and Gamma variants are in the U.S., but we don’t know if they’ll replace Delta. We have to monitor these variants to evaluate whether they’ll become dominant players in the future.
Finally, mRNA technology appears to be the key to getting a rapid and effective vaccine out should a more resistant variant develop. People need to realize that the technology is not new. Other forms of mRNA pharmaceuticals have already been approved for use in the U.S., and mRNA vaccines are very safe. Millions and millions of doses have been administered, and the adverse event rate associated with these vaccines is exceedingly low.

Widespread vaccination is the best way to stop the spread of Delta and prevent the rise of other COVID-19 variants. Credit: John Cameron
Should vaccinated people be avoiding gatherings in general, like visiting family members or going to restaurants?
Even if you are vaccinated you still can carry the virus and spread the virus to those who are not immune either because they’re unvaccinated or because they cannot make an adequate immune response to the vaccine. If you know your family is all vaccinated and there is a low chance of carrying the virus to at-risk people, then it’s OK to visit.
Social distancing is still important when it comes to being with other people, especially if you do not know their vaccination status. It’s reasonable to go to restaurants, as long as you know that they’re not at full capacity and there is good ventilation. Eating outside, of course, is even better.
It’s also important to consider where you are going and what you are doing after attending a large gathering. If you’re going to be around someone who is immunocompromised, and you’ve been to an event where you do not know the vaccination status of those attending, you must take into consideration that you can carry as much virus in your throat and mouth as someone who has not been vaccinated and has no symptoms. The concern would be that you might spread that virus to immunocompromised or unvaccinated people even though you may not yourself be ill.
What is a key message from all of this?
So far, our vaccines appear to be holding efficacy. For Gamma and Delta, our vaccines still have good vaccine efficacy, but we don’t know what the vaccine efficacy will be with the next epidemic variant of SARS-CoV-2.
We know more people are being hospitalized with the Delta variant. It’s frightening, but we have been lucky that death rates in those who are vaccinated are much lower than reported before the vaccines were available.
We are still seeing a lot of Delta variant spread. Therefore, it’s so important that unvaccinated people practice social distancing, wear masks, use hand hygiene, and get vaccinated. Vaccination not only protects the individual but also protects children, elderly people, and those immunocompromised persons who may not have responded to the vaccine in the first place (i.e., cancer patients, persons who are on medications to suppress the immune system for autoimmune disorders, transplant recipients). We can’t care about just ourselves anymore. We have to care about all of humanity.





This Q&A is very helpful to folks who haven’t been involved in the constant new cycle about the virus. It does talk about the Delta variety, but not specifically why it’s so bad.
All the coronaviruses and all their variants have different protein spikes, with Delta having one that’s more efficient at getting around the vaccines. But the real problem is in the virus itself, not its protein shell, and why the most dangerous (MERS, SARS, and Covid-19) are so infectious. My independent research has found multiple one-in-a-million nucleotide sequence matches between all the coronaviruses and the human genome. Those sequences are the same as some of the loops of human tRNA. Using those loops and their amino acid code matches, viruses may be able to fool the nucleus membrane in cells to allow the virus to enter and associate with the human DNA, creating more opportunities for further infection. Our immune system may be compromised and may no longer be able to stop the virus and other diseases from attacking organs throughout the body. Vaccines that attack the virus protein shells while ignoring their contents are doomed to failure from the Darwin effect, but recognizing these loops suggests a possible approach to successful coronavirus vaccines. Only the infection process is considered in my work, not the innate virulence of the virus. For more info, check out this YouTube, Coronavirus – Using Your DNA Against You. https://www.youtube.com/watch?v=8dOIzD6ch8s
I was fully vaccinated and spent 2 weeks in the hospital. At home on Oxygen now, but much better! I’ve read way too many statistics which all seem very different. as in Phizer didn’t do very well preventing delta variant from keeping people out of the hospital. probably helped people recover but some stats I say, of those who died, 49% had been fully vaccinated. (deaths rates were much less than original covid though and I would encourage every adult to get vaccinated.)