Research led by the University of Bristol suggests that romosozumab, a new anti-osteoporosis drug, could potentially increase the risk of heart attack, despite its efficacy in reducing fracture risk in women with severe osteoporosis. The study, which used genetic data of approximately 34,000 individuals, indicated that lowering levels of sclerostin, the protein blocked by romosozumab, might lead to a 30% increased risk of heart attack, among other health risks.
The study analyzed the genetic data of nearly 34,000 people.
A study led by the University of Bristol, recently published in Arthritis & Rheumatology, highlights potential safety risks associated with a new anti-osteoporosis drug, romosozumab, currently offered by the NHS. The study examined genetic data from close to 34,000 individuals.
Romosozumab has been found to significantly decrease fracture risk in women suffering from severe osteoporosis. However, data from clinical trials indicate a potential increased risk of heart attacks linked to the drug. However, further research on this issue has yielded inconsistent results.
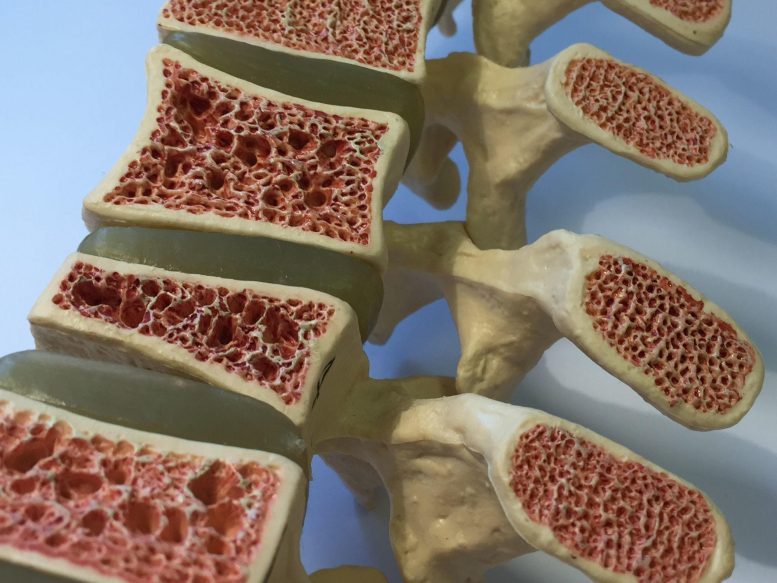
An international team, led by Bristol Medical School researchers, sought to investigate whether, having a genetic tendency towards lower circulating levels of sclerostin — a protein expressed from bone cells that inhibits bone formation— may increase the risk of heart attack. They propose that this mimics the effect of giving the drug romosozumab, which acts to stimulate bone formation and increase bone density by blocking sclerostin.
Jon Tobias, Professor of Rheumatology at Bristol Medical School: Translational Health Sciences at the University of Bristol, and one of the study’s lead authors, explained: “Osteoporosis commonly affects older people, particularly women, where bones become weaker and more liable to fracture. Romosozumab is a new type of drug that is highly effective at treating this condition by blocking the protein sclerostin, which is produced by bone cells and negatively impacts bone density. Administered as monthly injections, the drug helps to increase bone density and lower fracture risk.
“We wanted to predict whether romosozumab’s action in blocking sclerostin might lead to an increased risk of heart attack, by examining effects of a genetic tendency to lower levels of sclerostin, on the basis that this might reproduce some of the effects of administering the drug.”
The team applied a scientific technique called Mendelian randomization. This approach, which uses genetic variants as proxies for a particular risk factor, established whether having a genetic tendency to lower levels of sclerostin in the circulation increases a person’s risk of 15 diseases and risk factors related to atherosclerosis (hardening of the arteries). These included heart attack, stroke, type 2 diabetes, and high blood pressure.
Using genetic data on 33,961 European individuals, the team identified several genetic variants associated with lower levels of sclerostin. Their analyses suggested that lowering sclerostin levels might lead to a 30 percent increased risk of heart attack, as well as an increased risk of calcification of the arteries of the heart, hypertension, and type 2 diabetes, whereas no effect was seen on stroke risk. A genetic predisposition to lower sclerostin also led to lipid profiles that were more likely to cause atherosclerosis.
Professor Jon Tobias added: “Our findings suggest that individuals genetically predisposed to lower circulating levels of sclerostin have an increased risk of cardiovascular events, reinforcing the need for strategies to minimize any potential impact of treatment with sclerostin inhibitors on heart attack risk, some of which are already in place, such as avoidance in patients with previous cardiovascular problems.”
Reference: “Lowering of circulating sclerostin may increase risk of atherosclerosis and its risk factors: evidence from a genome-wide association meta-analysis followed by Mendelian randomization” by Jie Zheng, Ph.D., Eleanor Wheeler, Ph.D., Maik Pietzner, Ph.D., Till F.M. Andlauer, Ph.D., Michelle S. Yau, Ph.D., April E. Hartley, Ph.D., Ben Michael Brumpton, Ph.D., Humaira Rasheed, Ph.D., John P Kemp, Ph.D., Monika Frysz, Ph.D., Jamie Robinson, Ph.D., Sjur Reppe, Ph.D., Vid Prijatelj, Ph.D., Kaare M. Gautvik, MD, Ph.D., Louise Falk, MSc, Winfried Maerz, Ph.D., Ingrid Gergei, MD, Patricia A Peyser, Ph.D., Maryam Kavousi, Ph.D., Paul S. de Vries, Ph.D., Clint L. Miller, Ph.D., Maxime Bos, Ph.D., Sander W. van der Laan, Ph.D., Rajeev Malhotra, MD, MS, Markus Herrmann, Ph.D., Hubert Scharnagl, Ph.D., Marcus Kleber, Ph.D., George Dedoussis, Ph.D., Eleftheria Zeggini, Ph.D., Maria Nethander, MSc, Claes Ohlsson, Ph.D., Mattias Lorentzon, MD, Ph.D., Nick Wareham, Ph.D., Claudia Langenberg, Ph.D., Michael V. Holmes, Ph.D., George Davey Smith, MD, FRS and Jonathan H. Tobias, MD, PhD, 25 April 2023, Arthritis & Rheumatology.
DOI: 10.1002/art.42538
The study was funded by the University of Bristol’s Avon Longitudinal Study of Parents and Children (ALSPAC) and MRC Integrative Epidemiology Unit (IEU).









Y’all are “headline whores”…not even into the first third and: “However, data from clinical trials indicate a potential increased risk of heart attacks linked to the drug. However, further research on this issue has yielded inconsistent results.”