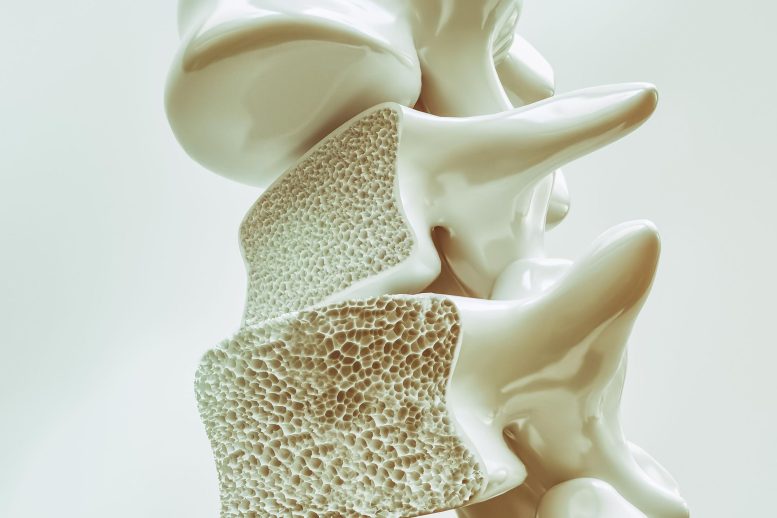
A 3D rendering of a cross-section of the spine showing bone loss due to osteoporosis. Osteoporosis is a progressive bone disease characterized by low bone density and increased risk of fractures, commonly affecting older individuals, particularly postmenopausal women. It is often asymptomatic until a fracture occurs, making early diagnosis and preventive measures crucial in managing this condition.
The Fracture Risk Assessment Tool (FRAX), frequently utilized in assessing fracture risk, incorporates self-identified race and ethnicity information. However, its performance in accurately determining the risk of major osteoporotic fractures among younger postmenopausal women across different racial and ethnic groups was found to be suboptimal.
On the other hand, the Osteoporosis Self-Assessment Tool (OST), which does not consider race and ethnicity, demonstrated excellent efficacy in identifying individuals with osteoporosis within each racial and ethnic category.
Background
The researchers sought to compare the ability of FRAX and OST to predict fracture risk in postmenopausal women aged 50 to 64 years in each of four racial/ethnic categories: Asian, Black, Latino, and white. Both tools are among those recommended by the U.S. Preventive Services Task Force to identify women within the younger age group who should undergo bone mineral density testing. The FRAX calculator requires the user to select one of those four racial/ethnic categories, but their inclusion in clinical risk prediction tools is controversial and the subject of much debate.
Methodology
Between May and August 2022, the researchers examined 10 years of follow-up data from nearly 67,200 younger postmenopausal participants in the Women’s Health Initiative for major osteoporotic fractures of the hip, spine, forearm, and shoulder. Of those women, nearly 5,600 experienced a fracture. The researchers assessed a subset of 4,600 participants for bone mineral density.
Impact
The U.S. version of FRAX, which requires race/ethnicity information, should not be routinely used to make screening decisions in younger postmenopausal women, the researchers write. Neither OST nor FRAX identified women who had a fracture during the subsequent 10 years. But OST is an excellent tool for identifying women with osteoporosis-level bone mineral density, which puts them at risk for fractures, while FRAX is not.
Commentary
“Identifying women with osteoporosis by bone density is the goal of screening because those women are potential candidates for osteoporosis drug therapy,” said Dr. Carolyn Crandall, professor of medicine in the division of general internal medicine and health services research at the David Geffen School of Medicine at UCLA and the study’s lead author. “For that purpose, OST performs better than FRAX, is simpler to use, and doesn’t require the inclusion of race or ethnicity information.”
Reference: “Race and Ethnicity and Fracture Prediction Among Younger Postmenopausal Women in the Women’s Health Initiative Study” by Carolyn J. Crandall, MD, MS, MACP, Joseph C. Larson, MS, John T. Schousboe, MD, Ph.D., JoAnn E. Manson, MD, DrPH, Nelson B. Watts, MD, John A. Robbins, MD, Peter Schnatz, DO, Rami Nassir, Ph.D., Aladdin H. Shadyab, Ph.D., Karen C. Johnson, MD, MPH, Jane A. Cauley, DrPH and Kristine E. Ensrud, MD, MPH, 22 May 2023, JAMA Internal Medicine.
DOI: 10.1001/jamainternmed.2023.1253
The Women’s Health Initiative program is funded by the National Institutes of Health’s National Heart, Lung, and Blood Institute.









Be the first to comment on "New Research Finds That Commonly Used Osteoporosis Tool Is Suboptimal"