
A large new study finds that higher blood levels of linoleic acid—a fat found in seed oils like soybean and corn—are linked to lower inflammation and better markers for heart and metabolic health, challenging popular claims that seed oils are harmful.
The researchers used blood markers instead of food diaries, making their results more robust, and observed that people with more linoleic acid in their plasma had lower blood sugar, insulin resistance, and inflammation. These findings suggest that omega-6 fats might actually be protective, not harmful, and call for further studies to test their benefits directly.
Omega-6 Fat Linked to Heart and Diabetes Risk
New research suggests that a type of fat found in common seed oils could actually protect against heart disease and type 2 diabetes. Scientists measured levels of linoleic acid, an omega-6 fatty acid, in people’s blood and found that higher amounts were linked to lower levels of inflammation and other risk factors tied to poor heart and metabolic health.
Linoleic acid is the most common omega-6 fat in our diets. It’s found in many plant-based foods and is especially abundant in vegetable oils like soybean and corn oil.
Controversy Around Seed Oils Addressed
“There has been increasing attention on seed oils, with some claiming these oils promote inflammation and raise cardiometabolic risk,” said Kevin C. Maki, Ph.D., adjunct professor at the Indiana University School of Public Health-Bloomington and chief scientist at Midwest Biomedical Research. “Our study, based on almost 1,900 people, found that higher linoleic acid in blood plasma was associated with lower levels of biomarkers of cardiometabolic risk, including those related to inflammation.”
Maki presented the findings at NUTRITION 2025, the flagship annual meeting of the American Society for Nutrition held in Orlando.
Evidence Aligns With Past Observational Studies
The new results are consistent with those from observational studies that have shown higher intake of linoleic acid to be associated with lower risks for type 2 diabetes and cardiovascular events, such as heart attacks and strokes.
“Although other studies have assessed relationships between linoleic acid and cardiometabolic risk factors, our study used objective biomarkers rather than diet records or food frequency questionnaires to assess linoleic acid intake,” said Maki. “We also measured a range of markers of inflammation and indicators of glucose metabolism.”
For the new study, the investigators performed a cross-sectional analysis on data from 1,894 people in an observational cohort focused on COVID-19. They found that higher levels of linoleic acid in plasma—indicative of dietary intake—were consistently associated with lower levels of risk factors for cardiovascular disease and type 2 diabetes.
Specific Biomarkers Show Clear Benefits
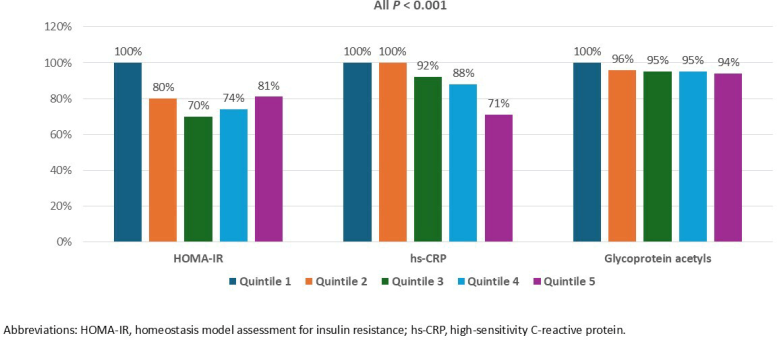
Specifically, study participants with higher linoleic acid showed lower levels of glucose and insulin as well as HOMA-IR, a biomarker of insulin resistance. They also had lower levels of inflammation biomarkers, including C-reactive protein, glycoprotein acetyls, and serum amyloid A.
“We saw consistent results across the different biomarkers measured,” Maki said. “People with higher levels of linoleic acid in their blood tended to have a healthier overall risk profile for heart disease and diabetes.”
The researchers say that their findings support the need for additional intervention studies to test whether increasing linoleic acid intake improves cardiometabolic risk factors and lowers the incidence of heart attacks, strokes, and type 2 diabetes. Next, they plan to investigate how different types of oils with varying fatty acid content affect cardiometabolic risk factors.
Meeting: NUTRITION 2025
Never miss a breakthrough: Join the SciTechDaily newsletter.
1 Comment
The reason high circulating levels of linoleic acid lowers inflammation and improves metabolic markers of health is because linoleic acid molecules displace arachidonic acid molecules from their positions in cell membranes. Norwegian animal science researchers explain how that works. “Because arachidonic acid (AA) competes with EPA and DHA as well as with LA, ALA and oleic acid for incorporation in membrane lipids at the same positions, all these fatty acids are important for controlling the AA concentration in membrane lipids, which in turn determines how much AA can be liberated and become available for prostaglandin biosynthesis following phospholipase activation. Thus, the best strategy for dampening prostanoid overproduction in disease situations would be to reduce the intake of AA, or reduce the intake of AA at the same time as the total intake of competing fatty acids (including oleic acid) is enhanced, rather than enhancing intakes of EPA and DHA only. Enhancement of membrane concentrations of EPA and DHA will not be as efficient as a similar decrease in the AA concentration for avoiding prostanoid overproduction.” https://pmc.ncbi.nlm.nih.gov/articles/PMC2875212/
There is, however, a downside to excessive linoleic acid consumption. “Fatty acid composition in the Western diet has shifted from saturated to polyunsaturated fatty acids (PUFAs), and specifically to linoleic acid (LA, 18:2), which has gradually increased in the diet over the past 50 y to become the most abundant dietary fatty acid in human adipose tissue. PUFA-derived oxylipins regulate a variety of biological functions. The cytochrome P450 (CYP450)–formed epoxy fatty acid metabolites of LA (EpOMEs) are hydrolyzed by the soluble epoxide hydrolase enzyme (sEH) to dihydroxyoctadecenoic acids (DiHOMEs). DiHOMEs are considered cardioprotective at low concentrations but at higher levels have been implicated as vascular permeability and cytotoxic agents and are associated with acute respiratory distress syndrome in severe COVID-19 patients.” https://pmc.ncbi.nlm.nih.gov/articles/PMC9060469/
Vijay P. Singh, MBBS, a gastroenterologist at the Mayo Clinic in Scottsdale, Arizona, and colleagues retrospectively looked at mortality and dietary and other factors in 15 COVID-19 patients, one of of whom died and seven of whom needed intensive care (ICU group). The rest were discharged home. They found that the ICU group had an early drop in serum calcium and albumin several days before ICU admission. Separately, on analyzing global COVID-19 mortality data and comparing it with 12 risk factors for mortality, they found unsaturated fat intake to be associated with increased mortality. This was based on the dietary fat patterns of 61 countries in the United Nations’ Food and Agricultural Organization database. Surprisingly, they found saturated fats to be protective. https://www.medpagetoday.com/reading-room/aga/lower-gi/86940
Clearly, one can reduce risk of heart attack by increasing linoleic acid consumption. However, if that means increasing risk of COVID-19 complications, that might not be a good idea.