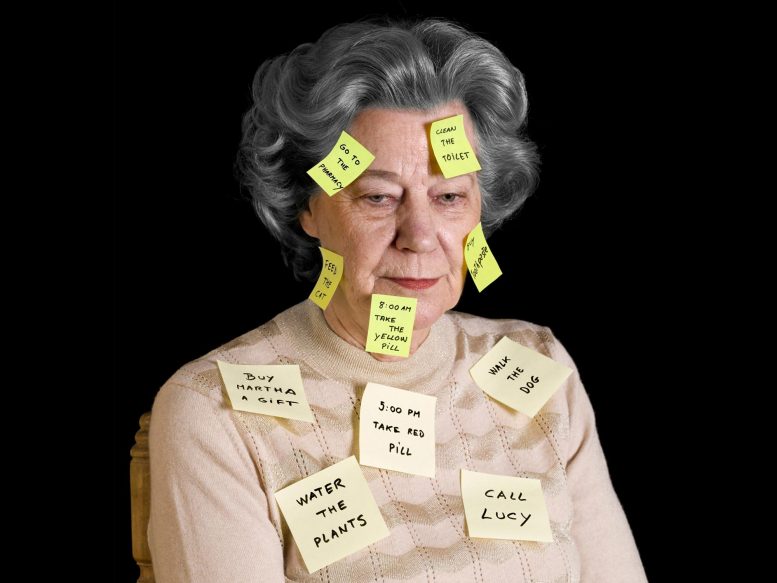
A study from Mass General Brigham indicates that inheriting Alzheimer’s disease risk from the maternal side is linked to higher amyloid levels in the brain, suggesting potential targets for early prevention in Alzheimer’s disease.
Study by Mass General Brigham indicates that considering sex-specific parental history may be crucial in identifying adults at an increased risk.
A recent study conducted by researchers from Mass General Brigham indicates that the parent from whom a person inherits Alzheimer’s disease risk may affect the likelihood of biological changes in the brain associated with the disease. The study assessed 4,400 cognitively unimpaired adults aged 65 to 85 and discovered that individuals with a family history of Alzheimer’s disease (AD) from their mother’s side or from both parents showed higher levels of amyloid in their brains. The findings were published in JAMA Neurology.
“Our study found if participants had a family history on their mother’s side, a higher amyloid level was observed,” said senior corresponding author Hyun-Sik Yang, MD, a neurologist at Mass General Brigham and behavioral neurologist in the Division of Cognitive and Behavioral Neurology at Brigham and Women’s Hospital. He is also a physician investigator of Neurology for the Mass General Research Institute.
Yang collaborated with other researchers from Mass General Brigham, as well as investigators from Vanderbilt and Stanford University. He said previous smaller studies have investigated the role family history plays in Alzheimer’s disease. Some of those studies suggested maternal history represented a higher risk of developing Alzheimer’s, but the group wanted to revisit the question with cognitively normal participants and access to a larger clinical trial data set.
Methodology and Participant Analysis
The team examined the family history of older adults from the Anti-Amyloid Treatment in Asymptomatic Alzheimer’s (A4) study, a randomized clinical trial aimed at AD prevention. Participants were asked about the memory loss symptom onset of their parents. Researchers also asked if their parents were ever formally diagnosed or if there was autopsy confirmation of Alzheimer’s disease.
“Some people decide not to pursue a formal diagnosis and attribute memory loss to age, so we focused on a memory loss and dementia phenotype,” Yang said.
Researchers then compared those answers and measured amyloid in participants. They found maternal history of memory impairment at all ages and paternal history of early-onset memory impairment were associated with higher amyloid levels in the asymptomatic study participants. Researchers observed that having only a paternal history of late-onset memory impairment was not associated with higher amyloid levels.
Gender Differences and Study Limitations
“If your father had early onset symptoms, that is associated with elevated levels in the offspring,” said Mabel Seto, PhD, first author and a postdoctoral research fellow in the Department of Neurology at the Brigham. “However, it doesn’t matter when your mother started developing symptoms — if she did at all, it’s associated with elevated amyloid.”
Seto works on other projects related to sex differences in neurology. She said the results of the study are fascinating because Alzheimer’s tends to be more prevalent in women. “It’s really interesting from a genetic perspective to see one sex contributing something the other sex isn’t,” Seto said. She also noted the findings were not affected by whether study participants were biologically male or female.
Yang noted one limitation of the study is some participants’ parents died young, before they could potentially develop symptoms of cognitive impairment. He said social factors like access to resources and education may have also played a role in when someone acknowledged cognitive impairment and if they were ever formally diagnosed.
“It’s also important to note a majority of these participants are non-Hispanic white,” Seto added. “We might not see the same effect in other races and ethnicities.”
Seto said the next steps are to expand the study to look at other groups and examine how parental history affects cognitive decline and amyloid accumulation over time and why DNA from the mother plays a role.
Reisa Sperling, MD, a co-author on the paper, principal investigator of the A4 Study and a neurologist at Mass General Brigham, said the findings could be used soon in clinical translation.
“This work indicates that maternal inheritance of Alzheimer’s disease may be an important factor in identifying asymptomatic individuals for ongoing and future prevention trials,” Sperling said.
Reference: “Parental History of Memory Impairment and β-Amyloid in Cognitively Unimpaired Older Adults” by Mabel Seto, Timothy J. Hohman, Elizabeth C. Mormino, Kathryn V. Papp, Rebecca E. Amariglio, Dorene M. Rentz, Keith A. Johnson, Aaron P. Schultz, Reisa A. Sperling, Rachel F. Buckley and Hyun-Sik Yang, 17 June 2024, JAMA Neurology.
DOI: 10.1001/jamaneurol.2024.1763
Disclosures: Yang has received personal fees from Genentech, Inc., outside the submitted work. Hohman serves on the Scientific Advisory Board for Vivid Genomics, outside the submitted work. Eli Lilly and Co. funded the A4 Study but had no direct influence in the submitted work.
This work was funded by the United States National Institutes of Health (K23AG062750, R01AG063689 U19AG010483, and DP2AG082342). The A4 Study is funded by NIH grants, Eli Lilly and Co, and several philanthropic organizations.







As a now eighty year old lay male with a family history of nearly subclinical non-IgE-mediated food allergies and dementia, who personally experienced temporary short-term memory problems along with my own self-discovered calcium deficiency in late 2010, I can state with some certainty the reason mothers are more likely to have Alzheimer’s disease is undiagnosed calcium deficiency, due at least in part to the extra demands of pregnancy for calcium for which standard blood serum testing is unreliable.
In conjunction with women also having higher incidents of osteoporosis than men, researchers should be testing for allergies, accurate calcium levels (e.g., ionic testing) and serum uric acid levels (resultant of allergy related low grade inflammation; affects calcium distribution in terms of optimal blood pH) in terms of prevention instead of looking for genetic causes in terms of cures and/or perpetual treatments.