Scientists may have uncovered a possible mechanism for why people with hypertension, diabetes, high cholesterol, or obesity have an increased chance of developing Alzheimer’s disease.
Alzheimer’s disease is the leading cause of dementia in older adults and the 7th most common cause of death in the United States according to the National Institute on Aging. It is a debilitating progressive illness that begins with mild memory loss and slowly destroys cognitive function and memory.
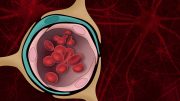
As the name implies, vascular diseases are conditions that affect your vascular system, which is your body’s network of blood vessels.
For more than 20 years, scientists have known that people with hypertension, diabetes, high cholesterol, or obesity have a higher likelihood of developing Alzheimer’s disease.
The conditions can all affect the brain, damaging blood vessels and leading to strokes. But the connection between vascular disease in the brain and Alzheimer’s has remained unexplained despite the intense efforts of researchers.
Now, a study led by researchers at Columbia University’s Vagelos College of Physicians and Surgeons has discovered a possible mechanism. The study found a gene called FMNL2 links cerebrovascular disease and Alzheimer’s and suggests changes in FMNL2 activity caused by cerebrovascular disease prevent the efficient clearance of toxic proteins from the brain, eventually leading to Alzheimer’s disease.
The finding could lead to a way to prevent Alzheimer’s in people with hypertension, diabetes, obesity, or heart disease.
“Not only do we have a gene, but we have a potential mechanism,” says senior author Richard Mayeux, MD, chair of neurology at Columbia and NewYork-Presbyterian/Columbia University Irving Medical Center. “People have been trying to figure this out for a couple of decades, and I think we have our foot in the door now. We feel there must be other genes involved and that we’ve just scratched the surface.”
Mayeux and his colleagues found FMNL2 in a genome-wide hunt designed to uncover genes associated with both vascular risk factors and Alzheimer’s disease. The search involved five groups of patients representing different ethnic groups.
One gene, FMNL2, stood out during the analysis. But what role it could possibly play was unclear. That’s when Caghan Kizil, PhD, a visiting associate professor at Columbia, leveraged his expertise with zebrafish as a model organism for Alzheimer’s disease.
FMNL2 and the blood-brain barrier
“We had this gene, FMNL2, that was lying at the interface between Alzheimer’s disease in the brain and cerebrovascular risk factors,” says Kizil. “So we had an idea that FMNL2 might operate in the blood-brain barrier, where brain cells meet the vasculature.”
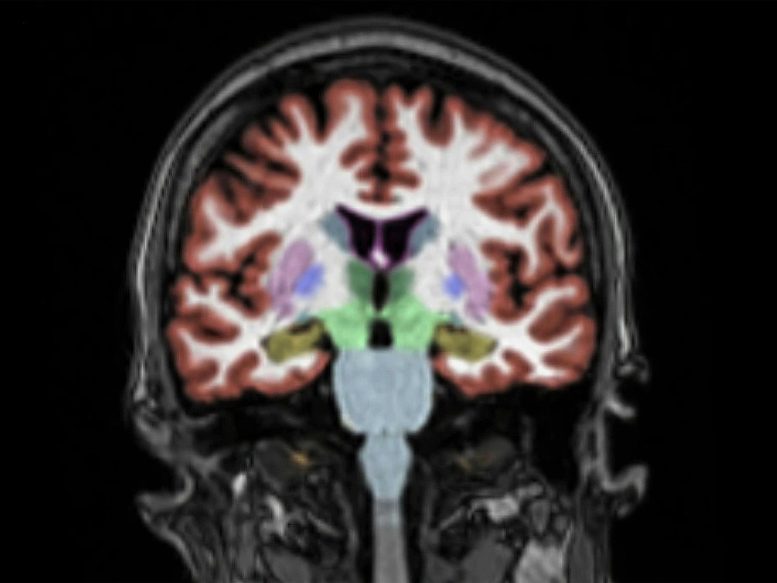
The blood-brain barrier is a semi-permeable, highly controlled border between capillaries and brain tissue that serves as a defense against disease-causing pathogens and toxins in the blood. Astrocytes, a specialized type of brain cell, compose and maintain the structure of the blood-brain barrier by forming a protective sheath around the blood vessel. This astrocyte sheath needs to loosen for the clearance of toxic amyloid—the aggregates of proteins that accumulate in the brain and lead to Alzheimer’s disease.
The zebrafish model confirmed the presence of FMNL2 in the astrocyte sheath, which retracted its grip on the blood vessel once toxic proteins were injected into the brain, presumably to allow for clearance. When Kizil and his colleagues blocked the function of FMNL2, this retraction did not occur, preventing clearance of amyloid from the brain. The same process was then confirmed using transgenic mice with Alzheimer’s disease.
The same process may also occur in the human brain. The researchers studied postmortem human brains and found increased expression of FMNL2 in people with Alzheimer’s disease, along with breach of the blood-brain barrier and retraction of the astrocytes.
Based on these findings, the researchers propose that FMNL2 opens the blood-brain-barrier—by controlling its astrocytes—and promotes the clearance of extracellular aggregates from the brain. And that cerebrovascular disease, by interacting with FMNL2, reduces the clearance of amyloid in the brain.
The team is currently in the process of investigating other genes that could be involved in the interplay between Alzheimer’s and cerebrovascular disease, which, along with FMNL2, could provide future approaches for drug development.
Reference: “FMNL2 regulates gliovascular interactions and is associated with vascular risk factors and cerebrovascular pathology in Alzheimer’s disease” by Annie J. Lee, Neha S. Raghavan, Prabesh Bhattarai, Tohid Siddiqui, Sanjeev Sariya, Dolly Reyes-Dumeyer, Xena E. Flowers, Sarah A. L. Cardoso, Philip L. De Jager, David A. Bennett, Julie A. Schneider, Vilas Menon, Yanling Wang, Rafael A. Lantigua, Martin Medrano, Diones Rivera, Ivonne Z. Jiménez-Velázquez, Walter A. Kukull, Adam M. Brickman, Jennifer J. Manly, Giuseppe Tosto, Caghan Kizil, Badri N. Vardarajan and Richard Mayeux, 24 May 2022, Acta Neuropathologica.
DOI: 10.1007/s00401-022-02431-6
Richard Mayeux, MD, is the Gertrude H. Sergievsky Professor of Neurology, Psychiatry and Epidemiology, director of the Gertrude H. Sergievsky Center, and co-director of the Taub Institute for Research on Alzheimer’s Disease and the Aging Brain at Columbia University.
The research was supported by the National Institutes of Health (grants RF1AG054023, R01AG067501, RF1AG066107, R01AG072474, P30AG10161, R01AG15819, R01AG17917, U01AG61356, R01AG036836, and U01AG046152); a Taub Institute Schaefer Research Scholar Award; the German Center for Neurodegenerative Diseases; and TAME-AD (The Thompson Family Foundation Program for Accelerated Medicine Exploration in Alzheimer’s Disease and Related Disorders of the Nervous System).
All authors: Annie J. Lee (Columbia), Neha S. Raghavan (Columbia), Prabesh Bhattarai (Columbia and German Center for Neurodegenerative Diseases), Tohid Siddiqui (German Center for Neurodegenerative Diseases), Sanjeev Sariya (Columbia), Dolly Reyes-Dumeyer (Columbia), Xena E. Flowers (Columbia), Sarah A.L. Cardoso (Columbia), Philip L. De Jager (Columbia), David A. Bennett (Rush University Medical Center), Julie A. Schneider (Rush University Medical Center), Vilas Menon (Columbia), Yanling Wang (Rush University Medical Center), Rafael A. Lantigua (Columbia), Martin Medrano (Pontificia Universidad Catolica Madre y Maestra, Dominican Republic), Diones Rivera (Universidad Pedro Henriquez Urena, Dominican Republic), Ivonne Z. Jiménez-Velázquez (University of Puerto Rico School of Medicine), Walter A. Kukull (University of Washington), Adam M. Brickman (Columbia), Jennifer J. Manly (Columbia), Giuseppe Tosto (Columbia), Caghan Kizil (Columbia and German Center for Neurodegenerative Diseases), Badri N. Vardarajan (Columbia), and Richard Mayeux (Columbia).






For more than 85 years mainstream medical research has been handicapped by its failure to recognize and research Dr. Arthur F. Coca’s kind of individually practically harmless ambiguous, brief and very-very mild (subclinical; non-IgE-mediated) food allergy reactions as true allergies, since the early 1930s. For more than 40 years they, and I (as a victim) have been handicapped by their failure to adequately question the US FDA’s illegal ‘GRAS’ approval of toxic added ‘cultured’ MSG for expanded use as an alleged ‘flavor enhancer’ in 1980 and for more than 30 years they’ve been additionally handicapped by their failure to recognize the added-allergy/MSG-related origin of the US obesity/diabetes epidemic in 1990 (CDC/NCHS data). With family histories of allergies, multiple cases of dementia and now two personal histories (e.g. 2009-2010 and 2021-2022) of temporary short term memory problems, beginning with the FDA in October of 2005 about obesity I’ve been sharing my now senior lay American adult male findings with more than a thousand more authoritative, more qualified and/or more resourceful professional others for more than 16 years, albeit mostly in-vain. Obviously, to me, ‘failure to communicate’ is another supreme failure of mainstream medicine which, Covid-19 or not, contributes to thousands of premature American fatalities every day. I doubt you/they will ever learn that any of that from a zebrafish or transgenic mouse FMNL2 gene.
Would this include people affected by migraine headaches? Migraines are vascular in nature and occur in the brain. I’m 50 and I’m experiencing cognitive dysfunction that I think isn’t normal for my age, too many “senior moments” for my liking. Just wondering.
Hello Tracey, I’m no doctor, I don’t get migraines and I’m not sure your comment was directed at me, personally, but I do believe migraines could be resultant of undiagnosed food allergies aggravated long-term with toxic FDA approved food additives. I was first diagnosed with high blood pressure in 1992 at age 48, after about a decade of ignorantly increasingly ingesting added MSG since 1980. A more likely substance, I think, would be aspartame artificial sweetener, FDA approved in 1981. In my lay opinion the three most obvious common symptoms of Dr. Arthur F. Coca’s (my) kind of chronic allergy reactions long term are obesity, so-called male pattern baldness and eyeglasses for myopia. And, it could be environmental substances (e.g. Dr. Lisa Nagy, Martha’s Vineyard, via her website). In late 2010 while suffering fatigue and short term memory problems (minimally) I discovered experimentally at-home that I was deficient in calcium (minimally) and online that standard blood serum testing for calcium is unreliable because, in the absence of an adequate dietary supply the body moves calcium around to try to maintain the blood at an optimal pH, slightly alkaline. Ionic testing for calcium might be better and a high serum level of uric acid might indicate-for my kind of allergies. I hope you find this helpful.
I was prescribed Verapimil for my migraines in1994 by a very smart and sensitive Dr. Michel in Sacramento. I had migraines for 20 years! Since the Verapamil I have not had a headache. I am now 84.6 yo.and a very active senior.
Also need to look at the dirty super 7 genes for epigenetic fixes which eliminate the need for pharmaceutical symptom suppression therapy at all!
Yeah, idiots, if you’re going to pop off don’t be general. It’s everything untreated. Put a percentage on all statements. I don’t think long serving nuns would appreciate you tossing them in some asinine study put together by abject clowns who, apparently can barely string two thoughts together. You been hitting the bottle a little too heavy? Talk about Alzheimers!