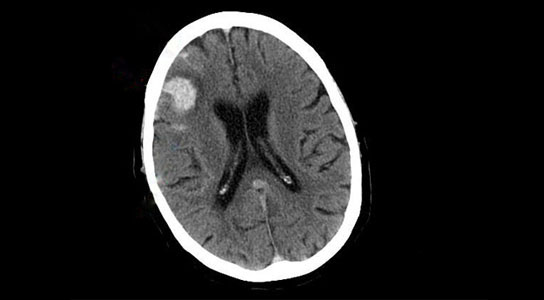
MIT researchers have developed a way to monitor pressure inside the brains of patients with injuries such as the bleeding seen in this CT scan. Credit: Lucien Monfils/wikipedia
Researchers in MIT’s Research Laboratory of Electronics have developed a new strategy to help treat and measure brain pressure without the invasive drilling of the skull. By using a computer model of how blood flows through the brain, doctors can calculate brain pressure from arterial blood pressure and an ultrasound measurement of the velocity of blood flow through the brain, allowing them to measure changes in pressure over time.
Brain tumors and head trauma, including concussions, can elevate pressure inside the skull, potentially crushing brain tissue or cutting off the brain’s blood supply. Monitoring pressure in the brains of such patients could help doctors determine the best treatment, but the procedure is so invasive — it requires drilling a hole through the skull — that it is done only in the most severely injured patients.
That may change with the development of a new technique that is much less risky. The method, described in the April 11 issue of Science Translational Medicine, could allow doctors to measure brain pressure in patients who have suffered head injuries that are milder, but would benefit from close monitoring.
Developed by researchers in MIT’s Research Laboratory of Electronics (RLE), the new technique is based on a computer model of how blood flows through the brain. Using that model, the researchers can calculate brain pressure from two less invasive measurements: arterial blood pressure and an ultrasound measurement of the velocity of blood flow through the brain.
With this approach, changes in brain pressure can be monitored over time, alerting doctors to problems that might build up slowly.
Under pressure
Pressure in the brain, also known as intracranial pressure (ICP), can rise due to the presence of excessive fluid (blood or cerebrospinal fluid), a brain tumor or swelling of the brain.
To measure this pressure, neurosurgeons drill a hole in the skull and insert a catheter into the brain tissue or a fluid-filled cavity in the brain. In all but the most critically ill patients, the risk of infection or damage to the brain outweighs the benefits of this procedure, says study co-author George Verghese, the Henry Ellis Warren Professor of Electrical Engineering at MIT.
“There’s a much larger patient population for whom physicians would like this measurement, but the invasiveness stops them from obtaining it,” says Verghese, whose lab focuses on using computer models of human physiology to interpret patient data.
In his PhD thesis, Faisal Kashif, who is now a postdoc in Verghese’s lab and the lead author on the paper, developed a computer model that relates arterial blood pressure and blood flow through the brain to pressure in the brain. The flow of blood through the brain is caused by the difference in pressure between the blood entering the brain and pressure inside the brain (ICP). Therefore, using Kashif’s model, ICP can be calculated from the flow and the pressure of blood entering the brain.
The pressure of blood entering the brain is not directly measurable, so the MIT team used radial arterial pressure, taken by inserting a catheter at the wrist, as a proxy for that measurement. They then used their model of blood flow to compensate for the difference in location.
Peripheral arterial pressure can also be measured continuously and noninvasively by using a finger cuff similar to the arm cuff commonly used to measure blood pressure. The researchers are now investigating whether data obtained this way is accurate enough to use in their model.
Validation
The researchers verified the accuracy of their technique using data collected several years ago by collaborator Marek Czosnyka at Cambridge University in the U.K., from patients with traumatic brain injury. This was one of the few data sets that included all the measurements they needed, along with the proper time stamps. Czosnyka sent the data on radial arterial blood pressure and ultrasound blood flow velocity to the MIT team, which then ran the numbers through their model and came up with an estimated ICP. They then sent that back to Czosnyka for comparison.
Their results were slightly less accurate than those obtained with the best invasive procedures, but comparable to other invasive procedures that are still in clinical use, and to some less invasive techniques that have been tried.
“It’s a holy grail of clinical neurosurgery to find a noninvasive way to measure pressure,” says James Holsapple, chief of neurosurgery at Boston Medical Center. “It would be a big step if we could get our hands on something reliable.”
The new MIT approach shows promise, Holsapple says, adding that an important next step is to incorporate the technology into a system that would be easy for hospital staff to use and could record data over many hours or days.
The MIT team, along with co-author Vera Novak of Beth Israel Deaconess Medical Center (BIDMC) in Boston, is now collaborating with doctors at BIDMC to test their approach on patients in the neurosurgical intensive care unit.
“It’s still at the validation stage. To convince people that this works, you need to build up more [data] than we currently have,” Verghese says. “Our hope is that once it’s been validated on additional sorts of patients, where you’re able to show that you can match what the invasive measurement is, people will have confidence in starting to apply it to patients who are currently not getting monitored. That’s where we see the big potential.”
Thomas Heldt, a research scientist in RLE and senior author of the paper, says that once the data collection and model are well-established, the team hopes to test different patient populations — such as athletes with concussions, or soldiers who have experienced explosions — to come up with ways to determine the extent of injury and when it is not yet safe for an athlete or soldier to return to the field.
Another potential application is monitoring astronauts during and after long space flights. NASA has observed signs of elevated ICP in some of these astronauts, and is now seeking new ways to measure it.
Reference: “Model-Based Noninvasive Estimation of Intracranial Pressure from Cerebral Blood Flow Velocity and Arterial Pressure” by Faisal M. Kashif, George C. Verghese, Vera Novak, Marek Czosnyka and Thomas Heldt, 11 April 2012, Science Translational Medicine.
DOI: 10.1126/scitranslmed.3003249








Be the first to comment on "Computer Model Monitors Brain Pressure Without Invasive Drilling"