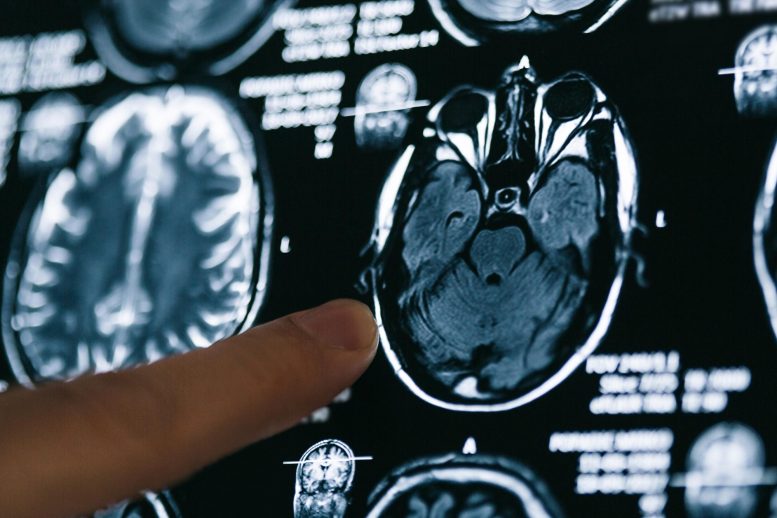
SARS-CoV-2 infection can lead to various neurological and psychiatric symptoms, suggesting the virus may affect the brain and nervous system.
The cluster of neurological symptoms associated with SARS-CoV-2 infection, the virus that causes COVID-19, suggests the virus can enter the brain and affect neural function. New findings were presented at Neuroscience 2021, the annual meeting of the Society for Neuroscience and the world’s largest source of emerging news about brain science and health.
Although much of the attention on COVID-19 centers on its respiratory effects, the virus has significant neurological manifestations as well. Many people infected with SARS-CoV-2 report neurological and psychiatric symptoms, including headache, loss of sense of smell and taste, hallucinations, vivid dreams, depression, fatigue, “brain fog,” and even seizures or stroke. These symptoms suggest the virus is capable of reaching the brain and may also affect other areas of the nervous system. Even for those who initially recover, many will experience lingering cognitive or neurological problems for months post-infection.
These new findings show:
- An analysis of human brain tissue identified two proteins, NRP1 and furin, that may mediate SARS-CoV-2 entry into human brain cells (Ashutosh Kumar, All India Institute of Medical Sciences-Patna).
- Studies of rhesus monkeys reveal how SARS-CoV-2 invades and spreads through the brain (John H. Morrison, University of California, Davis).
- In mice, peripheral nerve cells that transmit touch and pain information to the central nervous system are susceptible to SARS-CoV-2 infection, offering a possible route to infect the brain (Jonathan D. Joyce, Virginia Tech).
- COVID-19 can result in a prolonged effect on brain wave patterns for at least four months, but these differences may resolve by seven months post-infection (Allison B. Sekuler, Rotman Research Institute, McMaster University, and University of Toronto).
“We are just beginning to understand the central nervous system manifestations of COVID-19,” said Rita Balice-Gordon, the chief executive officer of Muna Therapeutics, an early-stage company working on novel therapeutics for neurodegenerative diseases. “The research presented today adds important new information about the neurobiological mechanisms underlying COVID’s effects on cognition and behavior.”
This research was supported by national funding agencies including the National Institutes of Health and private funding organizations. Find out more about COVID-19 and the brain on BrainFacts.org.
Nervous System Manifestations of COVID-19 Press Conference Summary
- SARS-CoV-2 coronavirus disease 2019 (COVID-19) can affect the brain, where it contributes to neurological and psychiatric symptoms.
- New research examines how SARS-CoV-2 enters and spreads in the brain and how the virus affects brain function.
NRP1 and Furin as Putative Mediators of SARS-CoV-2 Entry in Human Brain Cells
Ashutosh Kumar, Abstract P322.04
- The key receptor known to mediate SARS-CoV-2 entry into host cells is undetectable in human brain tissue.
- Researchers investigated potential alternate receptors through which SARS-CoV-2 could enter brain cells.
- A study of gene transcript and protein expression in human brain tissue revealed widespread expression of two molecules, NRP1 and furin, which previous studies have linked to SARS-CoV-2 entry into host cells.
- The findings suggest NRP1 and furin may mediate SARS-CoV-2 entry into human brain cells.
Sensory and Autonomic Ganglia of the Peripheral Nervous System Are Permissive to Infection With SARS-CoV-2 and May Provide an Avenue of Neural Invasion in K18-hACE2 Mice
Jonathan D. Joyce, Abstract P322.06
- Neurological symptoms of COVID-19 impact the central nervous system (headache, brain fog, cardiorespiratory failure) and the peripheral nervous system (pain, tingling, and loss of sensation in the fingers and toes), indicating both the brain and peripheral nerves are affected.
- Studies in mice reveal the peripheral nerve clusters that transmit touch and pain information to the brain and spinal cord can be infected by SARS-CoV-2, both in wild-type mice and those engineered to express the main ACE2 receptor the virus uses to enter human cells.
- These findings suggest infection of theses peripheral nerves may explain some of the symptoms of COVID-19 associated with altered sensation.
- These findings also suggest these peripheral nerves may offer an alternative route via which SARS-CoV-2 can enter the brain, as these nerves connect to parts of the brain associated with COVID-19 disease, including the limbic system and cardiorespiratory centers.
Transsynaptic Spread Combined With Glia-Driven Neuroinflammatory Response Orchestrate the Neuro-Invasive Potential of SARS-CoV-2 in an Aged Monkey Model of COVID-19
John H. Morrison, Abstract P318.02
- Among rhesus monkeys infected with SARS-CoV-2, aged, diabetic monkeys showed more viral presence in the brain and more aggressive spreading than young, healthy animals.
- Preliminary results suggest SARS-CoV-2 enters the brain via olfactory neurons and spreads to interconnected regions, leading to extensive inflammation within seven days of infection.
- This nonhuman primate model provides the opportunity to investigate the mechanisms of viral infection in the brain and evaluate potential therapeutic strategies aimed at protecting the brain.
Resting State Electroencephalography (rsEEG) In Individuals Recovering From COVID-19 After Self-isolation: A Longitudinal Observational Study
Allison B. Sekuler, Abstract P322.05
- This study is a part of NEUROCOVID-19, a project using comprehensive neurological and psychological evaluation of individuals with different clinical courses to investigate chronic brain effects of COVID-19.
- Resting-state electroencephalogram (EEG) data were collected from individuals who self-isolated at home and tested positive for COVID-19 and individuals who self-isolated but tested negative, with an initial visit about four months post-infection and a follow-up three months later.
- At the initial assessment, individuals positive for COVID-19 demonstrated different brainwave patterns than those who tested negative, with some of these effects still present at the three-month follow-up.
- The results suggest COVID-19 can have a lasting impact on brain function over at least seven months. Because the results are analogous to those seen in aging and mild cognitive impairment, the effect of COVID-19 on the brain may have implications for the future prevalence and detection of dementia.






Be the first to comment on "COVID-19 Can Infect Nerve Cells and Cause a Range of Neurological and Psychiatric Symptoms"