
A new study calls into question the dogma behind Alzheimer’s drug trials.
The study discovered that as Alzheimer’s disease progresses, brain levels of enzymes that regulate DNA-folding decrease.
Researchers from the University of Pittsburgh, McGill University, and Harvard University found that, in contrast to earlier research, the levels of brain enzymes that control DNA folding drop as Alzheimer’s disease worsens. Their findings were recently published in the journal Nature Communications.
These dogma-challenging findings show that decreased levels of Histone Deacetylase I (HDAC I), one of the enzymes that control how DNA is packaged inside the cell’s nucleus, are associated with the negative effects of misfolded beta-amyloid and tau proteins and Alzheimer’s disease-associated cognitive decline. These results were verified across two independent cohorts of live patients with Alzheimer’s disease as well as on post-mortem brain tissues.
Importantly, the new findings imply that using HDAC inhibitors—drugs that reduce HDAC levels and are presently being tested in clinical trials for mild Alzheimer’s disease—may be harming rather than benefiting patients.
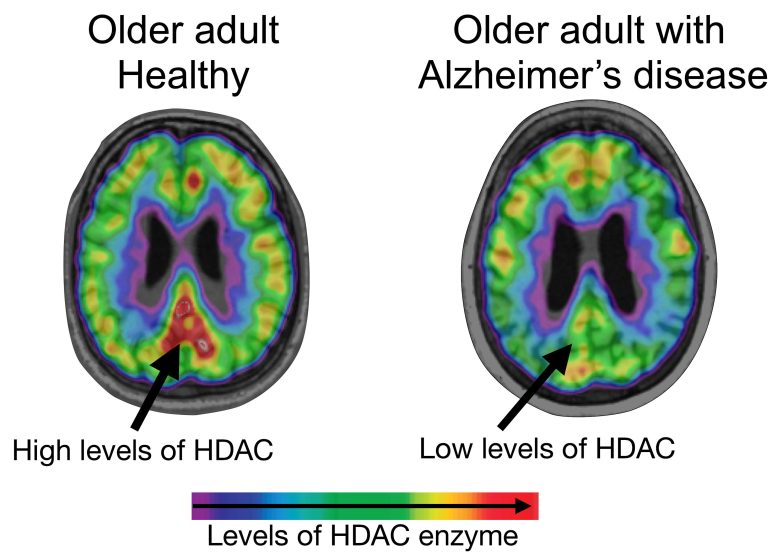
HDAC levels are reduced in the brains of older adults with Alzheimer’s disease compared to healthy older adults. Credit: Tharick Pascoal
“Approximately one-third of elders who have brain amyloid pathology do not develop Alzheimer’s disease,” said lead author Tharick Pascoal M.D. He is also an assistant professor of psychiatry and neurology at Pitt’s School of Medicine. He continues, “Now we have evidence of another factor that dictates whether or not the disease will progress further, and it is related to how the brain environment can affect the expression of our genes.”
Alzheimer’s disease is a deadly neurodegenerative disease that typically affects the elderly but begins decades before symptoms appear. Forty-four million people live with Alzheimer’s disease or associated dementia. Alzheimer’s patients develop cognitive impairments over time, including memory loss and difficulty thinking and speaking, due to the formation of plaques of misfolded beta-amyloid and tangled strands of tau proteins, which induce nerve cell death and brain tissue damage.
However, amyloid and tau disorders are just one piece of the complex picture. Over the last few decades, researchers have started to focus on additional processes—neuroinflammation and changes in the chemical environment of the brain cells—and how these might impact the development of the condition.
One of these processes is known as epigenetic histone modification. A cell may adjust the efficiency with which genetic information is translated into templates for new proteins by modifying how DNA is folded within its nucleus—whether it is tightly wrapped around protein barrels called histones or hung in looser threads. This permits the cell to swiftly and reversibly modify the way our genes operate and react to changes in the environment without changing the DNA sequence itself.
In the long quest to develop safe, effective therapies that stave off cognitive decline and reverse disease progression, a subtype of enzymes that drive epigenetic modifications—HDACs—emerged as promising targets for new Alzheimer’s therapies.
HDACs carry on a chemical reaction that encourages tighter packing of DNA molecules into condensed bundles and restricts biosynthesis of new proteins in response to environmental cues.
Earlier studies on post-mortem brain samples reported that levels of HDACs in the brains of patients with Alzheimer’s increase as the disease progresses. High levels of HDACs were thought to restrict the brain’s ability to produce new functional proteins that make up critical cell components and, therefore, contribute to memory loss and cognitive decline.
The new paper, however, challenges the status quo and adds another piece to an already confusing picture. The loss of HDAC I might be mechanistically linked with the emergence of beta-amyloid and tau pathologies—which, as Pascoal and colleagues showed in their previous paper, are intertwined with brain tissue inflammation and drive Alzheimer’s disease progression—and precede cognitive changes that accompany the disease.
To ensure that their findings represented the real picture across a diverse patient pool, researchers ran two parallel but entirely independent studies at McGill University in Canada and Massachusetts General Hospital, enrolling 94 participants in total. The two sites did not communicate throughout the study period and presented their results unaware of the other group’s findings.
Using a selective molecular tracer called [11C]Martinostat, researchers showed that HDAC I levels were greatly reduced in the brains of people with Alzheimer’s disease compared to non-Alzheimer’s controls, specifically in regions buried deep inside the brain’s core – hippocampus and the midline – as well as in the brain’s temporal cortex.
Analyses showed that reduced HDAC I in areas of the brain that are most susceptible to Alzheimer’s disease-associated degenerative changes corresponded to higher beta-amyloid and tau burden. It also predicted progressive neurodegeneration and cognitive decline over a two-year period.
While researchers are confident that the rigorous processes that govern clinical trial design ensure the highest standards of patient safety, they warn that efforts to test HDAC inhibitors might be misdirected. Instead, they say, the field needs to further explore the relationship between HDAC activation and disease progression and home in on which specific class of HDACs—out of a total of 18—plays a key role in Alzheimer’s disease-related brain pathology.
Still, the scientists are optimistic.
“The good news is that, by nature, epigenetic processes are changeable,” said Pascoal. “There is a lot of hope for future treatments, and a combination of anti-amyloid therapies with drugs that can rescue the loss of HDACs holds a lot of promise.”
Reference: “[11C]Martinostat PET analysis reveals reduced HDAC I availability in Alzheimer’s disease” by Tharick A. Pascoal, Mira Chamoun, Elad Lax, Hsiao-Ying Wey, Monica Shin, Kok Pin Ng, Min Su Kang, Sulantha Mathotaarachchi, Andrea L. Benedet, Joseph Therriault, Firoza Z. Lussier, Frederick A. Schroeder, Jonathan M. DuBois, Baileigh G. Hightower, Tonya M. Gilbert, Nicole R. Zürcher, Changning Wang, Robert Hopewell, Mallar Chakravarty, Melissa Savard, Emilie Thomas, Sara Mohaddes, Sarah Farzin, Alyssa Salaciak, Stephanie Tullo, A. Claudio Cuello, Jean-Paul Soucy, Gassan Massarweh, Heungsun Hwang, Eliane Kobayashi, Bradley T. Hyman, Bradford C. Dickerson, Marie-Christine Guiot, Moshe Szyf, Serge Gauthier, Jacob M. Hooker, and Pedro Rosa-Neto, 19 July 2022, Nature Communications.
DOI: 10.1038/s41467-022-30653-5
The study was funded by the Alzheimer’s Association, the Weston Brain Institute, Canadian Institutes of Health Research, the Fonds de Recherche du Quebec–Sant, and the National Institutes of Health.




Be the first to comment on "New Study Calls Into Question Widely-Held Alzheimer’s Beliefs"