
Acute Radiation Dermatitis is a skin condition typically experienced by individuals undergoing radiation therapy, especially in cancer treatments. This skin reaction, which can vary from mild redness and itchiness to severe burns and skin breakdown, occurs due to damage inflicted on the skin cells by ionizing radiation.
A recent study conducted at the Montefiore Einstein Cancer Center has demonstrated that a low-cost antibacterial treatment regimen can prevent acute radiation dermatitis.
Acute radiation dermatitis (ARD), is a condition commonly found in those undergoing cancer radiation treatment, affecting as many as 95% of patients. This condition is marked by symptoms such as redness, soreness, itching, or peeling of the skin. More severe instances may result in considerable swelling and painful skin ulcers, significantly impacting the quality of life of the patient. However, our understanding of why ARD occurs remains limited, and there are no widely adopted, standardized methods for preventing its severe form.
Researchers at Montefiore Einstein Cancer Center (MECC) have found that many cases of ARD involve a common skin bacterium and that a simple, low-cost treatment can prevent severe cases, potentially setting a new standard of care for people undergoing radiation therapy.
Their findings were reported in two papers recently published in JAMA Oncology. Each year, 10 million people are treated with radiation therapy to reduce the size of their tumors.
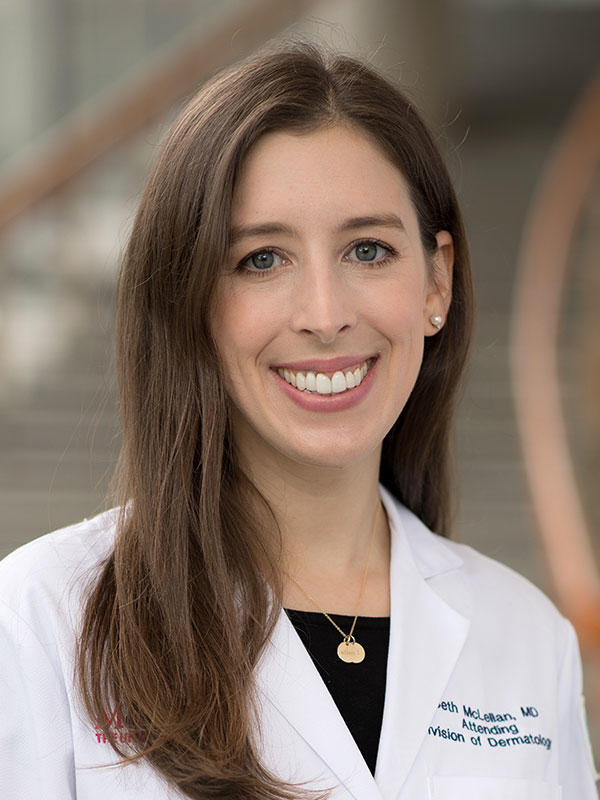
Dr. Beth McLellan senior author of the two studies. Credit: Albert Einstein College of Medicine
”Until now, ARD was assumed to result simply from the skin being burned by the radiation, which meant that not much could be done to prevent it,” said Beth N. McLellan, M.D. director, supportive oncodermatology at Montefiore Einstein Cancer Center, chief of the division of dermatology at Montefiore Health System and Albert Einstein College of Medicine, and senior author of the two studies. “The readily available treatment we’ve developed and clinically tested could potentially save hundreds of thousands of people each year in the U.S. from severe ARD and its excruciating side effects.”
Identifying the Source
Staphylococcus aureus (SA) bacteria, often shortened to “staph,” typically live harmlessly on the skin, often in the nose and armpits. But, they can cause infections if the skin is broken by a cut. Radiation weakens the skin’s structure at the treatment site and can result in infection by allowing SA to break through the skin’s outer layer. Courses of radiation therapy—routinely requiring daily treatments over several weeks—increase the risk of skin infection to occur.
Since SA is implicated in common skin disorders that lead to a breakdown in the skin such as eczema, Dr. McLellan and her colleagues reasoned that the bacteria might also play a role in ARD. In one of the JAMA Oncology studies, the MECC researchers enrolled 76 patients undergoing radiation therapy for cancer. Bacterial cultures were collected from patients before and after radiation treatment, from three different body sites: inside the nose, from skin in the radiated area, and from skin on the side of the body not exposed to radiation.
Before treatment, approximately 20% of patients tested positive for SA but did not have an active infection. Following treatment, 48% of those patients who developed severe ARD tested positive for the presence of SA, compared with only 17% of patients who developed the mildest form of the condition. Many patients with SA on their skin also tested positive for nasal SA, suggesting that SA from the nose might be infecting the skin.
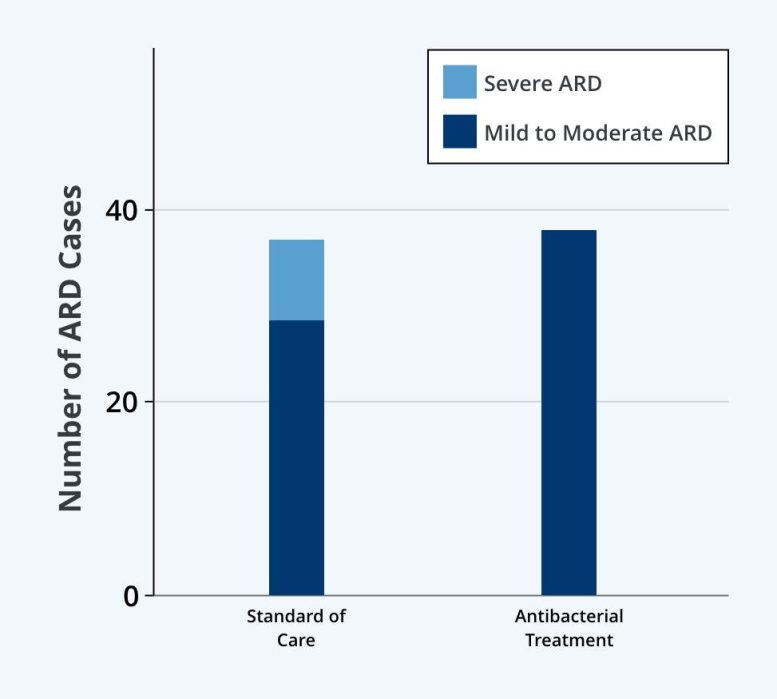
A new study in JAMA Oncology found that a simple antibacterial treatment prevents severe cases of radiation dermatitis (ARD): No patients in the treatment group developed severe ARD, while severe ARD affected 23% of patients treated with the current standard of care. (Mild to moderate ARD = Grade < 2; severe ARD = Grade > 2-MD). Credit: Courtesy Albert Einstein College of Medicine
“This study clearly showed that SA plays a major role in ARD,” said Dr. McLellan. “The good news is we have a lot of tools to fight this bacteria. In a second study, we tested a topical antibacterial drug combination we thought would be effective and easy for people to use.”
Preventing Severe ARD
The second study enrolled 77 patients undergoing radiation therapy, all but two of whom had breast cancer. Participants were randomized to receive either the standard of care at MECC (normal hygiene and moisturizing treatment such as Aquaphor), or the experimental antibacterial regimen. This treatment involved using the body cleanser chlorhexidine along with mupirocin 2% nasal ointment twice a day for five days, every other week, throughout their radiation treatment.
Although more than half the patients treated with the antibacterial regimen developed mild-to-moderate ARD, no patients developed moist desquamation—the most severe type of ARD that causes the skin to break down and develop sores—and no patients experienced adverse effects from the treatment. In contrast, severe ARD affected 23% of participants receiving the standard of care.
“Our regimen is simple, inexpensive, and easy so we believe it should be used for everyone undergoing radiation therapy, with no need to first test individuals for SA,” said Dr. McLellan. “I expect this will completely change protocols for people undergoing radiation therapy for breast cancer.”
Dr. McLellan also noted: “Like most of our trials at MECC, a majority of our participants were Black and Hispanic members of our community, meaning this protocol is generalizable and effective for people of different races and ethnicities. This is especially important because people with darker skin types are more likely to develop severe ARD.”
References: “Bacterial Decolonization for Prevention of Radiation Dermatitis – A Randomized Clinical Trial” by Yana Kost, Alana Deutsch, Karolina Mieczkowska, Roya Nazarian, Ahava Muskat, H. Dean Hosgood, Juan Lin, Johanna P. Daily, Nitin Ohri, Rafi Kabarriti, Kosaku Shinoda and Beth N. McLellan, 4 May 2023, JAMA Oncology.
DOI: 10.1001/jamaoncol.2023.0444
“Association of Staphylococcus aureus Colonization With Severity of Acute Radiation Dermatitis in Patients With Breast or Head and Neck Cancer” by Yana Kost, Alexandra K. Rzepecki, Alana Deutsch, Mathew R. Birnbaum, Nitin Ohri, H. Dean Hosgood, Juan Lin, Johanna P. Daily, Kosaku Shinoda and Beth N. McLellan, 4 May 2023, JAMA Oncology.
DOI: 10.1001/jamaoncol.2023.0454







Oh really? Hmmm…so I’m not a “conspiracy theorist” when I tell YOU that PROBIOTICS are the “answer’ to a LOT of things….EVEN heavy doses of gamma, EXTREMELY heavy doses even, like the ‘demon core’ did to researchers in the 1940’s can INSTANTLY be resolved, by the answer I JUST gave you!
You’re NOT supposed to know that, so you’re easily “controlled” by “MAD” pacts….
What do probiotics have to do with this? Do you put probiotics on your skin? The outer layer of your skin is dead, anything you eat to enhance your flora is unlikely to do anything about bacteria on your skin.
There is evidence that the superantigen of Staphylococcus aureus is responsible for causing type 2 Diabetes. When applied to the skin of rabbits, they become diabetic in one study. And obese people have more Staphylococcus aureus, suggesting that might be the link. Here they say Blacks and Hispanics are more likely to get this strong reaction. That suggests one more piece of evidence may be higher rates of Staphylococcus aureus on the skin in Blacks and Hispanics, leading to more cases of Diabetes. Of course, this is a hypothesis. Scientists would have to show that Blacks and Hispanics actually have more Staphylococcus aureus on their skin, as I am merely speculating that, that is why they are having more cases of this strong reaction.
I think it would be a good idea for everyone to do this skin sterilization procedure, not just people undergoing this radiation procedure. I did the skin part with chlorhexidine about 8 months ago. I’ll have to see about getting the nose stuff. I am not advising. I am just guessing. I only did it once. Well, I did it a second time, just on my feet and ankles. They did it several times. I may have to do it more, for it to do what I was hoping: to prevent diabetes.
My idea could backfire, and result in a strain chlorhexidine resistant Staph. Also, presumably there are beneficial bacteria on the skin as well. It would be nice to restore them.