
Schizophrenia is a severe mental illness that affects how a person thinks, feels, and behaves. The symptoms of schizophrenia can make it difficult to participate in usual, everyday activities, and people with schizophrenia may seem like they have lost touch with reality.
Scientists identify an autoantibody that may cause schizophrenia in some individuals.
Researchers from Tokyo Medical and Dental University (TMDU) have discovered that some people with schizophrenia have autoantibodies—which are made by the immune system and recognize the body’s own proteins, rather than outside threats such as viruses or bacteria—against a protein that’s important for communication between brain cells called NCAM1. The patients’ autoantibodies also caused schizophrenia-related behaviors in mice. This discovery may improve the diagnosis and treatment of a subset of patients with schizophrenia.
Schizophrenia is a disorder that affects how people act, think, and perceive reality. It is often very difficult to treat because it has many different causes and symptoms. In a study published recently in the journal Cell Reports Medicine, researchers from Tokyo Medical and Dental University (TMDU) have identified an autoantibody—a protein that is produced by the immune system to attach to a specific substance from the individual’s own body, rather than to a foreign substance like a virus or bacteria—in some patients with schizophrenia. Notably, they also found that this autoantibody, when injected into mice, caused schizophrenia-like behaviors and changes in the brain.
When considering possible autoantibodies that might cause schizophrenia, the scientists had a specific protein in mind. Previous research has suggested that neural cell adhesion molecule (NCAM1) may have a role in the development of schizophrenia. NCAM1 helps cells in the brain talk to one another via specialized connections known as synapses.
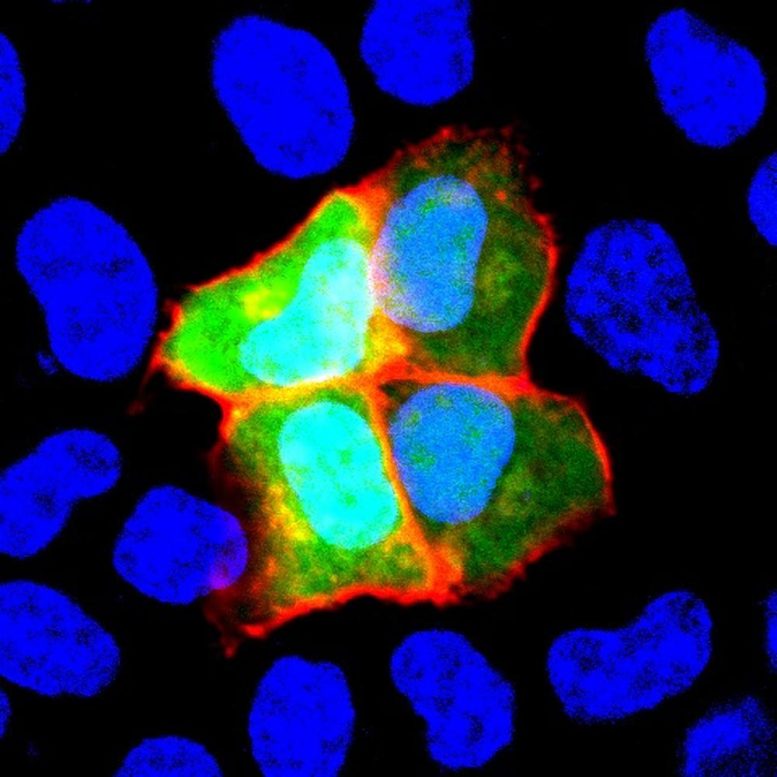
NCAM1 is induced only in green cells (HeLa cells). Serum from patients with anti-NCAM1 autoantibody react only to green cells (framed in red). Credit: Department of Psychiatry and Behavioral Sciences, TMDU
“We decided to look for autoantibodies against NCAM1 in around 200 healthy controls and 200 patients with schizophrenia,” explains lead author of the study Hiroki Shiwaku. “We only found these autoantibodies in 12 patients, suggesting that they may be associated with the disorder in just a small subset of schizophrenia cases.”
The researchers didn’t stop there—they wanted to know whether these autoantibodies could cause any changes that commonly occur in schizophrenia, so they purified autoantibodies from some of the patients and injected them into the brains of mice.
“The results were impressive,” says Hidehiko Takahashi, senior author. “Even though the mice only had these autoantibodies in their brains for a short time, they had changes in their behavior and synapses that were similar to what is seen in humans with schizophrenia.”
Specifically, mice with the patient autoantibodies had cognitive impairment and changes in their regulation of the startle reflex, which are both seen in other animal models of schizophrenia. They also had fewer synapses and dendritic spines, which are structures that are important for the connections between brain cells, and are also affected in schizophrenia.
Given that schizophrenia can present very differently among patients and is often resistant to treatment, the results of this study are promising. If schizophrenia is indeed caused by autoantibodies against NCAM1 in some patients, this will lead to important improvements in their diagnosis and treatment.
Reference: “Autoantibodies against NCAM1 from patients with schizophrenia cause schizophrenia-related behavior and changes in synapses in mice” by Hiroki Shiwaku, Shingo Katayama, Kanoh Kondo, Yuri Nakano, Hikari Tanaka, Yuki Yoshioka, Kyota Fujita, Haruna Tamaki, Hironao Takebayashi, Omi Terasaki, Yukihiro Nagase, Teruyoshi Nagase, Tetsuo Kubota, Kinya Ishikawa, Hitoshi Okazawa and Hidehiko Takahashi, 19 April 2022, Cell Reports Medicine.
DOI: 10.1016/j.xcrm.2022.100597
Funding: Ministry of Education, Culture, Sports, Science and Technology, JAPAN, Tokyo Biochemical Research Foundation, SENSHIN Medical Research Foundation








There are many causes of schizophrenia the recent research has shown that schizophrenia manifests after gaps in certain regions of the brain start forming. Holes in the brain in the visual and auditory centers. These holes can be formed in many ways, autoimmune is just one of those ways. You shouldn’t stop looking there. Nerve cells die off for a number of reason not enough energy, way too much activity (like how a marathoner looks like they’re about to die when they cross the finish line if they kept running they eventually would die some neurons go through that), many things can cause metabolic distress triggering cell suicide such as nuerotransmitter imbalances (which actually can be made worse by her current antipsychotic treatment, because they drastically reduce the amount of dopamine and or serotonin your nerve cells produce causing metabolic distress and cell suicide, particularly in people who don’t need this medication or for whom this type of medication is the incorrect treatment. New research has pointed to a protein that might help these individuals, I think that’s a lot better place to start then turning the switch on your most essential neurotransmitters.
There are many causes of schizophrenia the recent research has shown that schizophrenia manifests after gaps in certain regions of the brain start forming. Holes in the brain in the visual and auditory centers. These holes can be formed in many ways, autoimmune is just one of those ways. You shouldn’t stop looking there. Nerve cells die off for a number of reason not enough energy, way too much activity (like how a marathoner looks like they’re about to die when they cross the finish line if they kept running they eventually would die some neurons go through that), many things can cause metabolic distress triggering cell suicide such as nuerotransmitter imbalances (which actually can be made worse by her current antipsychotic treatment, because they drastically reduce the amount of dopamine and or serotonin your nerve cells produce causing metabolic distress and cell suicide, particularly in people who don’t need this medication or for whom this type of medication is the incorrect treatment. New research has pointed to a protein that might help these individuals, I think that’s a lot better place to start than turning the switch on your most essential neurotransmitters. Also you might have wanted to choose a more sensitive picture depicting the despair and angst of schizophrenia. What you have here is a caricature- these people are suffering, not demonic.