A new treatment for Parkinson’s disease is undergoing clinical trials, building on successful preliminary studies with non-human primates at the University of Wisconsin–Madison. This novel approach involves transplanting dopaminergic neuronal progenitor cells into the brain, a method refined through collaboration between researchers and Aspen Neuroscience. Initial results are promising, paving the way for potential breakthroughs in the management of Parkinson’s symptoms.
A clinical trial has begun to offer a new treatment to people with Parkinson’s disease, following a study by University of Wisconsin–Madison scientists. This study, conducted on non-human primates, confirmed that the therapeutic delivery method is safe and feasible.
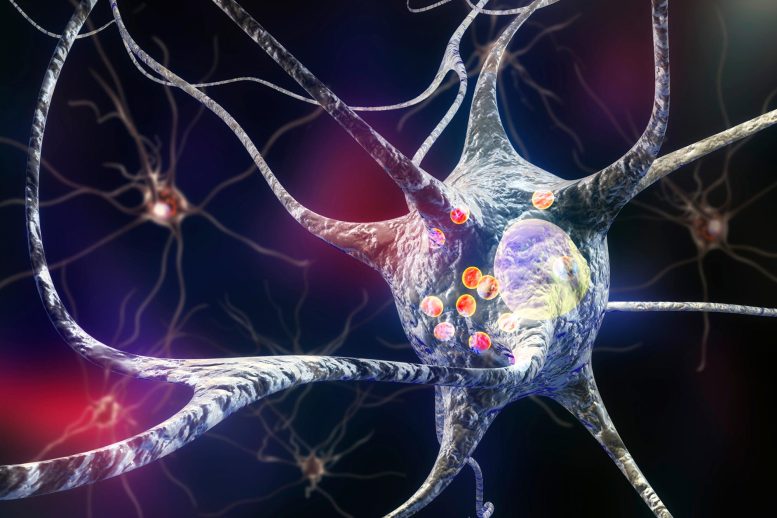
Parkinson’s disease damages neurons in the brain that produce dopamine, a brain chemical that transmits signals between nerve cells. The disrupted signals make it progressively harder to coordinate even simple movements and cause rigidity, slowness, and tremors that are the disease’s hallmark symptoms. Patients are typically treated with drugs like L-DOPA to increase dopamine production. Although the drugs help many patients, they present complications and lose their effectiveness over time.
Researchers at the Wisconsin National Primate Research Center successfully grafted brain cells called dopaminergic neuronal progenitor cells into the brains of cynomolgus macaque monkeys. California-based Aspen Neuroscience provided the cells, grown from multiple lines of human induced pluripotent stem cells, along with key pieces of the equipment for delivering them to specific parts of the brain.
“By the time of diagnosis, it is common for people with Parkinson’s to have lost the majority of dopaminergic neurons, leading to progressive loss of motor and neurological function,” explains Edward Wirth III, an expert in cell therapies, study co-author and Aspen’s chief medical officer. “To replace these lost cells, we must target a very specific area of the brain with a high degree of surgical precision. Utilizing the latest advances in intraoperative MRI guided techniques, the patient’s new cells are transplanted, a few microliters at a time, to the exact area where they are most needed.”
Autologous Cell Transplants
Working with potential cell therapies in pursuing treatments for Parkinson’s disease is a particular specialty of the team at Marina Emborg’s lab and their primate center colleagues.
“Using autologous cells, a patient’s own cells, avoids the need to use immunosuppression to keep the patient’s body from rejecting or attacking the graft,” says Emborg, a UW–Madison professor of medical physics. “Aspen has developed the technological methods for manufacturing, for quality control, that makes it feasible at scale to make autologous cells and get them to the patients.”
The researchers’ results in non-human primates, which supported Aspen’s successful Investigational New Drug application to the Food and Drug Administration to begin human trials, were published in the Journal of Neurosurgery.
“This study was an important step in our work to bring the promise of a cell-replacement therapy to people with Parkinson’s disease,” says Andrés Bratt-Leal, study co-author, Aspen Neuroscience co-founder and senior vice-president of research and development. “The results were instrumental in opening our first-in-human trial and informing how we deliver patients’ own cells to them in the study.”
Moving Towards Human Trials
The UW–Madison scientists, led by Parkinson’s researcher Emborg, took up the Aspen-funded work fresh off their own success (published in 2021) reversing Parkinson’s symptoms in monkeys by grafting neurons grown from the monkeys’ own cells, called an autologous transplant.
The 2021 study, using cells grown by UW–Madison stem cell researcher Su-Chun Zhang, added new dopamine-producing neurons to each animal’s brain through injections guided in real-time by MRI to an area of the brain called the putamen. Dopamine production increased dramatically, as did the monkeys’ motor skills. At the same time, symptoms of depression and anxiety were reduced.
The new study was designed to test the delivery of Aspen’s human cells. Wirth and Aspen scientists worked with Emborg’s team to bridge the monkey-to-human application. While Emborg’s previous study administered cells to the putamen through the top of the skull, the Aspen study examined cell administration through the back of the skull — an angle that could allow surgeons to reach their target with fewer insertions of the apparatus that delivers the new cells into the brain.
“The core idea is to decrease the risk of infection, the trauma, the surgical time the patient spends under anesthesia,” Emborg says. “The fewer tracks you have to follow through the brain, the better for all of that.”
Six monkeys received grafts of the human neurons through two paths in each side, or hemisphere, of their brains, with more cells deposited on one side of the brain than the other. A control group of three animals underwent the procedure without the cell delivery.
“In tissue samples taken seven and 30 days after the procedures, we found the grafted cells persisted in five of the animals,” Emborg says.
The researchers confirmed the presence of Aspen’s human neurons in the monkeys’ brains, finding more cells in the hemispheres that were injected with a higher dose, more cells in the 30-day tissue samples compared to the seven-day samples, and the presence of a protein produced by young neurons working to integrate with neighboring cells — all signs the cells grafts were successful.
It was a true collaboration, according to Emborg — between the Aspen scientists, her lab, and the Wisconsin National Primate Research Center veterinarians and staff — to validate the company’s procedures and equipment before study co-author Paul Larson, a neurosurgeon at Banner – University Medical Center Tucson and professor of neurosurgery at the University of Arizona College of Medicine – Tucson, began Aspen’s first-in-human trial with people with Parkinson’s in April.
The work done to refine the logistics, surgical equipment, and techniques in the animal procedures will inform the way patients in the human trial receive and recover from the new therapy, providing hope for those struggling with a debilitating disease.
“Our results were all so exciting,” Emborg says. “And then, when I saw they had been able to begin with a human patient this spring, I just had tears in my eyes.”
Reference: “Preclinical evaluation of transaxial intraputaminal trajectory for enhanced distribution of grafted cells in Parkinson’s disease” by Marina E. Emborg, Anthony Mancinelli, Julia C. Colwell, Alexandra D. Zinnen, Bruce Pape, Kevin Brunner, Viktoriya Bondarenko, Casey Fitz, Jennifer Coonen, Viktorie Menna, Kerri Fuchs, Nancy Schultz-Darken, Heather A. Simmons, Ha Tran, Paul Larson, Miles Olsen, Sam Hurley, Andres M. Bratt-Leal, Edward Wirth III, Jeanette M. Metzger, 26 July 2024, Journal of Neurosurgery.
DOI: 10.3171/2024.4.JNS24367






I am a medical anthropologist researcher of brain diseases, and I have tears in my eyes, too. These monkeys were tortured, sticking needles into their brains for 30 days. These researchers are psychopaths. According to the link in the article above to the press release from the torturers, “A neurotoxin was administered — a common practice for inducing Parkinson’s-like damage for research — and Emborg’s lab evaluated the monkeys monthly to assess the progression of symptoms. “We evaluated through observation and clinical tests how the animals walk, how they grab pieces of food, how they interact with people…” This is not Parkinson’s, but a poisoned monkey brain. These monkeys were abused, depressed, anxious, and the people doing this to them cannot justify this cruelty in any way.
To study Parkinson’s you need to study people who get it. Why does Parkinson’s develop in the first place? You can’t tell this from monkeys given nerve poison. See my article The Psychopathology of Animal Researchers . https://www.academia.edu/38646799/The_Psychopathology_of_Animal_Researchers_Vivisectors_