
A team from the University of Virginia School of Medicine has discovered that improper calcium signaling in the mitochondria of certain immune cells contributes to chronic inflammation that accelerates aging. They propose that enhancing calcium uptake in these cells could help to slow down age-related diseases. The findings are published in the scientific journal Nature Aging.
University of Virginia School of Medicine researchers have discovered a key driver of chronic inflammation that accelerates aging. That finding could let us slow the clock to live longer, healthier lives, and may allow us to prevent age-related conditions such as deadly heart disease and devastating brain disorders that rob us of our faculties.
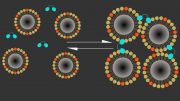
So what drives this harmful inflammation? The answer is improper calcium signaling in the mitochondria of certain immune cells. Mitochondria are the power generators in all cells, and they rely heavily on calcium signaling.
Implications of the Findings
The team at UVA Health, under the leadership of Bimal N. Desai, PhD, found that the mitochondria in macrophages, a type of immune cell, lose their ability to absorb and utilize calcium as they age. They demonstrated that this issue leads to the chronic inflammation accountable for many health problems associated with old age.
The University of Virginia School of Medicine’s Bimal N. Desai, PhD, and colleagues have found a key trigger for “inflammaging” — inflammation that drives aging. Credit: Dan Addison, University of Virginia
The researchers propose that enhancing calcium uptake by these mitochondrial macrophages could deter this harmful inflammation and its severe consequences. Given that macrophages are present in all our body organs, including the brain, directing targeted drugs towards such “tissue-resident macrophages” may enable us to slow age-related neurodegenerative diseases.
“I think we have made a key conceptual breakthrough in understanding the molecular underpinnings of age-associated inflammation,” said Desai, of UVA’s Department of Pharmacology and UVA’s Carter Immunology Center. “This discovery illuminates new therapeutic strategies to interdict the inflammatory cascades that lie at the heart of many cardiometabolic and neurodegenerative diseases.”
The Inflammation of Aging – ‘Inflammaging’
Macrophages are white blood cells that play critical roles in our immune systems and, in turn, our good health. They swallow up dead or dying cells, allowing our bodies to remove cellular debris, and patrol for pathogens and other foreign invaders. In this latter role, they act as important sentries for our immune systems, calling for help from other immune cells as needed.
Scientists have known that macrophages’ effectiveness diminishes with age, but the reasons for this were previously unclear. Desai’s recent discovery provides some answers.
A Keystone Mechanism in Aging
Desai and his team say their research has identified a “keystone” mechanism responsible for age-related changes in the macrophages. These changes, the scientists believe, make the macrophages prone to chronic, low-grade inflammation at the best of times. And when the immune cells are confronted by an invader or tissue damage, they can become hyperactive. This drives what is known as “inflammaging” – chronic inflammation that drives aging.
Further, the UVA Health scientists suspect that the mechanism they have discovered will hold true not just for macrophages but for many other related immune cells generated in the bone marrow. That means we may be able to stimulate the proper functioning of those cells as well, potentially giving our immune systems a big boost in old age, when we become more susceptible to disease.
The Way Forward
Fixing “inflammaging” won’t be as simple as taking a calcium supplement. The problem isn’t a shortage of calcium so much as the macrophages’ inability to use it properly. But Desai’s new discovery has pinpointed the precise molecular machinery involved in this process, so we should be able to discover ways to stimulate this machinery in aging cells.
“This highly interdisciplinary research effort, at the interface of computational biology, immunology, cell biology, and biophysics, wouldn’t have been possible without the determination of Phil Seegren, the graduate student who spearheaded this ambitious project,” Desai said. “Now, moving forward, we need an equally ambitious effort to figure out the wiring that controls this mitochondrial process in different types of macrophages and then manipulate that wiring in creative ways for biomedical impact.”
Aging Findings Published
The researchers have published their findings in the scientific journal Nature Aging. The article is open access, meaning it is free to read.
Reference: “Reduced mitochondrial calcium uptake in macrophages is a major driver of inflammaging” by Philip V. Seegren, Logan R. Harper, Taylor K. Downs, Xiao-Yu Zhao, Shivapriya B. Viswanathan, Marta E. Stremska, Rachel J. Olson, Joel Kennedy, Sarah E. Ewald, Pankaj Kumar and Bimal N. Desai, 5 June 2023, Nature Aging.
DOI: 10.1038/s43587-023-00436-8
The research team consisted of Seegren, Logan R. Harper, Taylor K. Downs, Xiao-Yu Zhao, Shivapriya B. Viswanathan, Marta E. Stremska, Rachel J. Olson, Joel Kennedy, Sarah E. Ewald, Pankaj Kumar, and Desai. The scientists reported that they have no financial interests in the work.
The research was supported by the National Institutes of Health, grants AI155808, GM108989, GM138381, P30 CA044579 and T32 GM007055-46, and by the Owens Family Foundation.








Please send me details about this anti aging product
In 2011 I wrote both JACI (Journal of Allergy and Clinical Immunology) and The Lancet of my 2010 lay findings of Dr. Arthur F. Coca’s kind of food allergies aggravated with FDA approved food poisoning (e.g., only added ‘cultured-free’ monosodium glutamate [MSG], then, more now) causing me a calcium deficiency not indicated-for with standard blood serum testing for calcium (redirected by the body to try to maintain an optimal blood pH, about 7.3). Both professional publications declined to publish my lay findings. I’ve since learned it starts with chronic mild inflammation which causes the release of xanthine oxidase which breaks down into uric acid and free radicals, minimally. Great work, Dr. Desai, even if you are more than a decade behind the times and don’t yet to know of existing cheap and easy prevention (as opposed to costly research into future symptomatic treatments).