
Researchers have discovered that changes in gut microbiome, specifically a reduction in Clostridia bacteria due to antibiotics and a high-fat diet, can lead to sorbitol intolerance. This intolerance manifests as digestive upset from consuming sorbitol, a common sugar alcohol in various foods and products. They found that regulating gut oxygen levels with certain bacteria or drugs like mesalazine could restore the ability to digest sorbitol, suggesting a new treatment approach for sorbitol intolerance.
Gut microbes missing due to antibiotics and a high-fat diet may be responsible for ‘sorbitol intolerance’.
Scientists at UC Davis have discovered alterations in the gut microbiome that lead to difficulties in digesting sorbitol.
Sorbitol, a sugar alcohol, is used in sugar-free gum, mints, candy and other products. It is also found naturally in apricots, apples, pears, avocadoes, and other foods. At high levels, sorbitol can cause bloating, cramps, and diarrhea. For some people, even a small amount causes digestive upset, a condition known as sorbitol intolerance.
A new study with mice found that taking antibiotics, combined with a high-fat diet, reduced the number of Clostridia gut microbes, which can break down sorbitol. The findings were published in the journal Cell.
“Our research suggests that microbial sorbitol degradation normally protects the host against sorbitol intolerance. However, an impairment in the microbial ability to break down sorbitol causes sorbitol intolerance,” said Jee-Yon Lee, first author of the study. Lee is an assistant project scientist in the UC Davis Department of Medical Microbiology and Immunology.
How oxygen levels in the gut affect microbes
The researchers used metagenomic analysis to identify which gut bacteria have genes that make the enzyme that breaks down sorbitol. They also identified which of those gut bacteria were plentiful before — but not after — antibiotic treatment.
This analysis allowed them to zero in on gut microbes belonging to the class Clostridium. Clostridium are anaerobic, meaning they don’t like environments with oxygen.
The researchers found that after the mice were given antibiotics and fed a diet high in saturated fat, the cells lining the gut used less oxygen. This created a higher level of oxygen in the gut, decreasing Clostridia. Without enough Clostridia, sorbitol was not broken down in the gut.
The researchers performed several experiments to try to restore the gut bacteria so it could break down sorbitol again.
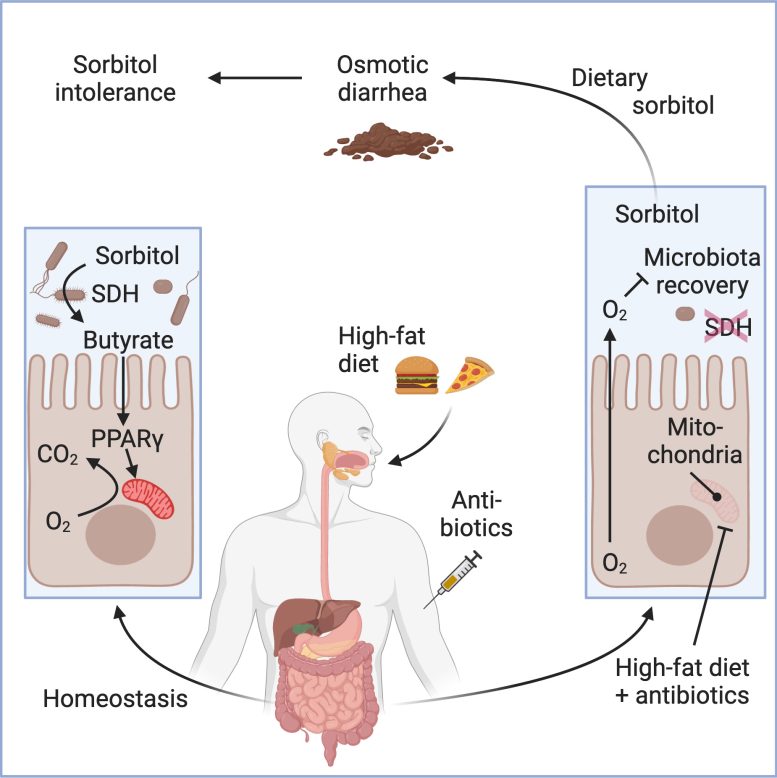
Taking antibiotics, combined with a high-fat diet, reduced the number of Clostridia gut microbes. Image generated with BioRender. Credit: UC Davis Health
In one, they fed the mice Anaerostipes caccae, a gut bacterium that produces butyrate. Butyrate is a short-chain fatty acid produced as part of the normal fermentation process in the gut. It enhances oxygen usage by the cells that line the gut, the epithelial lining, which reduces oxygen levels in the large intestine.
Regulating the oxygen level with Anaerostipes caccae restored the normal levels of Clostridia, which protected the mice from sorbitol-induced diarrhea, even after the butyrate-producing bacteria had been cleared from the mouse’s digestive system.
The researchers suggest that a drug used to treat ulcerative colitis, Crohn’s disease, and other inflammatory bowel diseases, mesalazine (5-aminosalicylate), may be a treatment for sorbitol intolerance in humans. Mesalazine, also known as mesalamine, functions similarly to the butyrate-producing bacteria, restoring the low oxygen levels in the intestine preferred by Clostridia.
“This discovery is crucial, given the prevalent use of sorbitol and similar sugar alcohols in the production of keto-friendly diet foods that are high in fat content,” Lee said. “It also highlights the importance of oxygen consumption by the epithelial lining in the intestines in maintaining a healthy balance of gut bacteria, especially Clostridia, for proper digestion of certain sugars.”
An important limitation of the study is that mice can tolerate much higher sorbitol levels than humans. Mice possess a cecum — a pouch in their digestive system that slows the flow of intestinal contents and helps digest carbohydrates, which may contribute to being able to better tolerate sorbitol. Clinical studies will be needed to test the hypothesis that mesalazine could treat sorbitol intolerance in humans.
“Our study provides a completely new starting point for approaches to diagnose, prevent, and treat sorbitol intolerance,” said Andreas Bäumler, senior author of the study. Bäumler is a distinguished professor and vice chair of research in the UC Davis Department of Medical Microbiology and Immunology.
Reference: “High fat intake sustains sorbitol intolerance after antibiotic-mediated Clostridia depletion from the gut microbiota” by Jee-Yon Lee, Connor R. Tiffany, Scott P. Mahan, Matthew Kellom, Andrew W.L. Rogers, Henry Nguyen, Eric T. Stevens, Hugo L.P. Masson, Kohei Yamazaki, Maria L. Marco, Emiley A. Eloe-Fadrosh, Peter J. Turnbaugh and Andreas J. Bäumler, 15 February 2024, Cell.
DOI: 10.1016/j.cell.2024.01.029
Co-authors include Connor Tiffany, Scott Mahan, Andrew Rogers, Henry Nguyen, and Hugo Masson of the UC Davis School of Medicine; Eric Stevens and Maria Marco of UC Davis; Matthew Kellom and Emiley A. Eloe-Fadrosh of Lawrence Berkeley National Laboratory; Kohei Yamazak of Kitasato University in Japan; and Peter Turnbaugh of UC San Francisco (UCSF) and Chan Zuckerberg Biohub.
The study was funded by the Kenneth Rainin Foundation.








Be the first to comment on "Does Sugar-Free Candy Give You Gas? Scientists Have Discovered Why"