In a study, a new HIV drug reduced viral replication and increased immune cells in individuals with advanced, drug-resistant HIV infection. Used in combination with existing HIV medications, the drug is a promising strategy for patients who have run out of effective treatment options, the researchers said.
The study, co-authored by Yale assistant professor of medicine Brinda Emu, M.D., was published in the New England Journal of Medicine.
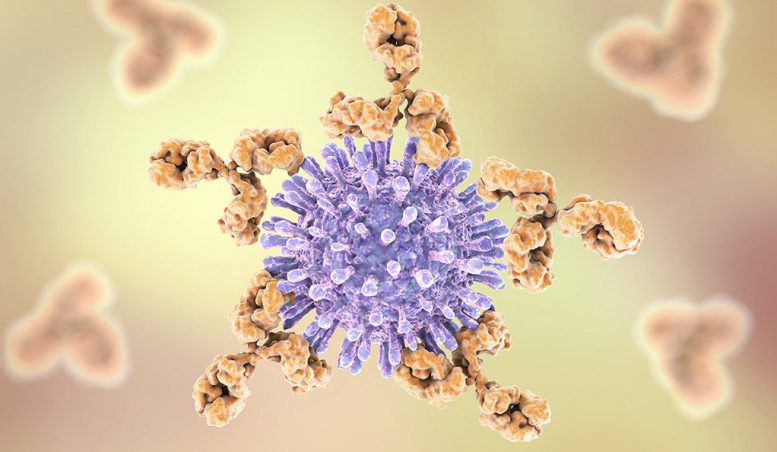
For some individuals with HIV, existing drug therapies fail to suppress the virus, leading to drug resistance and worsening disease. While several HIV drugs target the virus effectively, there has not been a new class of HIV drugs approved to combat the disease in a decade. In March 2018, the FDA approved ibalizumab, a drug that targets the primary receptor for HIV entry into immune cells known as CD4 T cells. This novel mechanism of action prevents HIV from entering target cells.
Multiple sites participated in the study, including Yale, enrolling patients with multi-drug-resistant HIV. Patients received a dose of ibalizumab, which is delivered intravenously, in addition to their failing regimen, for one week. After that period, they received ibalizumab in combination with optimized treatment regimens for six months.
The research team found that after one week on ibalizumab, the majority of the 40 patients (83%) enrolled in the study experienced a decrease in viral load, which refers to the amount of HIV detected in the blood. After 25 weeks, nearly half of the patients saw viral load suppression dip below the level of detection. The researchers also reported an increase in CD4 T cells, which are a marker for immune strength. A single individual experienced an adverse event, which was felt to be ibalizumab-related and resulted in withdrawal from the study, the researchers said.
The results were notable for this drug-resistant population of patients studied, said Emu: “These patients had extremely advanced HIV and resistant virus with limited options. To see viral suppression in a significant percentage of these patients at six months is heartening. The result represents a much-needed new mechanism of action for patients who have highly resistant HIV.”
As the first monoclonal antibody approved to treat HIV, ibalizumab is a promising option for individuals who have tried several other drug therapies. “It should be considered for patients that have multi-drug resistance given the efficacy seen in this study,” she noted.
Because of its novel mechanism, ibalizumab will not interact negatively with other medications. It is also delivered intravenously every two weeks and lasts longer than current HIV drugs, which are taken daily by mouth.
“It’s ushering in a whole class of medicine and a new mode of delivery for the treatment of HIV,” said Emu. “I look forward to discussions in the community about how such a therapy will fit into the current treatment paradigm for HIV infection.”
She added, “we must also keep in mind that ibalizumab was approved with a smaller number of patients treated than other medications due to the rarity of patients with multi-drug resistant HIV. As such, patients and providers must remain vigilant for side effects and adverse events.”
Other study authors are Walford Fessel, Shannon Schrader, Princy Kumar, Gary Richmond, Sandra Win, Steve Weinheimer, Christian Marsolais, and Stanley Lewis.
This study was supported by the FDA’s Orphan Products Clinical Trials Grants Program. All authors, including academic authors, and those of the sponsor, TaiMed Biologics, contributed to the writing and review of the manuscript. Disclosure forms (PDF) provided by the authors are available at the New England Journal of Medicine website.






Be the first to comment on "New HIV Therapy Boosts Immunity and Reduces Viral Replication"