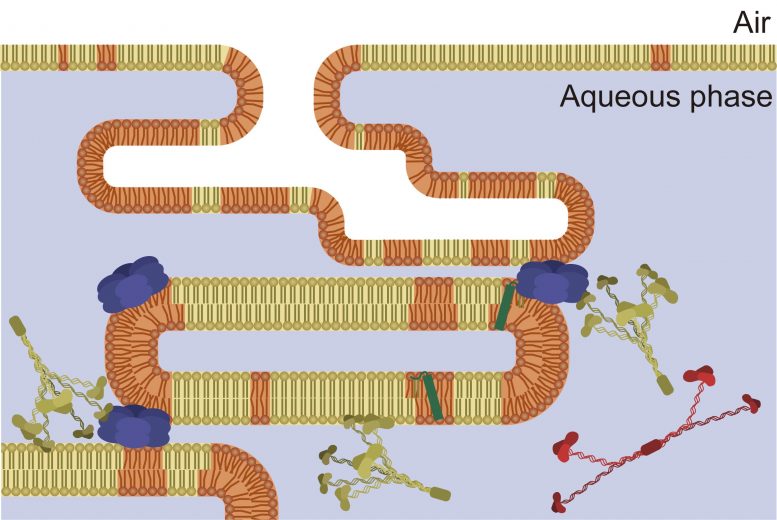
This drawing depicts surfactant (orange and yellow), which is a molecular layer at the interface of air and liquid in the lung that is essential for breathing. New research shows that temperatures used during therapeutic hypothermia improve surfactant’s activities. Credit: Image courtesy of Chiara Autilio and created by Alejandro Alonso
A new study reveals how lower temperatures improve the activity of surfactant, a molecular mixture that is essential for breathing. This indicates that therapeutic hypothermia is a potential treatment for acute respiratory distress syndrome, which affects a tenth of all intensive care unit patients.
A tenth of all intensive care unit patients worldwide, and many critical patients with COVID-19, have acute respiratory distress syndrome (ARDS). Therapeutic hypothermia, an intentional cooling of the body, has been suggested as a way to improve ARDS. New research by Chiara Autilio and colleagues in the lab of Jesus Perez-Gil at the Complutense University of Madrid shows not only how therapeutic hypothermia works in the lungs at the molecular level, but also why it could be successfully applied to ARDS. Autilio and her colleagues’ work was published in Nature Scientific Reports in January 2021 and will be presented on Tuesday, February 23 at the 65th Annual Meeting of the Biophysical Society to be held virtually.
Inside our lungs, surfactant is a molecular mixture that is essential for breathing. Premature babies are sometimes born without yet having developed surfactant and require emergency surfactant replacement treatments in order to breathe. But surfactant is also inactivated and broken up in adults with lung injuries or inflammation.
Because therapeutic hypothermia, a cooling of the body to about 33°C (or 91°F), has been used to improve breathing for some premature babies and for some kinds of cardiac arrest in adults, and some early studies have shown a benefit for ARDS, Autilio, and colleagues wanted to know if cooling could impact surfactant. They looked at the physics of isolated surfactant in their lab, and Autilio said, “unexpectedly, we found an improvement in surfactant activity at 33°C.”
The team found that at 33°C, the surfactant had lower surface tension, which could make it easier for oxygen to enter the lungs. They also found that the lower tension changed the activity of the molecules in the surfactant, which prevented surfactant from being disrupted by blood molecules, which can occur during lung injury. Their results indicate that “using therapeutic hypothermia could help people with acute respiratory distress syndrome to breathe.”
There are currently clinical trials underway in other labs, testing therapeutic hypothermia as a treatment for severe breathing problems associated with COVID-19, according to Autilio. And in the Perez-Gil lab at the Complutense University, “we are working to create a surfactant for adults, a surfactant that could work in the context of acute respiratory distress syndrome,” says Autilio.
Reference: “Molecular and biophysical mechanisms behind the enhancement of lung surfactant function during controlled therapeutic hypothermia” by C. Autilio, M. Echaide, A. Cruz, C. Mouton, A. Hidalgo, E. Da Silva, D. De Luca, B. Sørli Jorid and J. Perez-Gil, 12 January 2021, Scientific Reports.
DOI: 10.1038/s41598-020-79025-3









Be the first to comment on "Therapeutic Hypothermia: How Reducing Body Temperature Could Help 10% of All Intensive Care Patients"