Researchers at Edith Cowan University have found promising results from a trial combining an mRNA vaccine, tailored to individual tumor genetics, with conventional immunotherapy for high-risk melanoma patients. The results showed a significant increase in cancer-free survival rates and decreased disease recurrence, potentially marking a significant stride toward personalized cancer treatment.
Incorporating a personalized mRNA vaccine, designed to match an individual’s tumor genetics, into standard immunotherapy substantially boosts survival rates and reduces the recurrence of high-risk skin cancers in patients who have had these malignancies removed.
Global trials that could revolutionize cancer treatment and save countless lives are being led by scientists from Edith Cowan University (ECU).
Clinical Professor Adnan Khattak from ECU’s Centre for Precision Health recently unveiled the newest findings from these trials at the 2023 American Society of Oncology (ASCO) congress in Chicago. The ASCO congress, attracting more than 45,000 participants, is the largest cancer treatment conference worldwide.
Professor Khattak outlined how survival and disease recurrence rates among people who’d had high-risk skin cancers (melanomas) removed improved significantly when an mRNA vaccine tailored to suit an individual’s tumor genetics was added to common immunotherapy treatment.
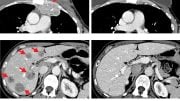
After 18 months, cancer-free survival among patients who received the vaccine and the immunotherapy treatment was 78.6 percent, compared to 62.2 percent of those who only received the immunotherapy.
Two years after treatment, only 22.4 percent of patients who had received the vaccine/immunotherapy combination had either died or seen a recurrence of the disease, which rose to 40 percent for the immunotherapy-only group.
Overall, after an average of two years, those who received the vaccine saw a 44 percent lower risk of death or melanoma returning to the same area of the body, and a 65 percent reduction in the risk of death or the cancer returning in a different area of the body.
Crucially, there was no significant increase in rates of adverse side effects.
Professor Khattak said the trial began as a way of trying to address the shortcomings of current treatments.
“The current standard of care is immunotherapy using an antibody known as pembrolizumab,” he said.
“There are two main issues: first, despite having active immunotherapy for stage three melanoma, about half of the patients will relapse at five years.
“And secondly, it’s a very crude approach: currently if I treat 10 new high-risk melanoma patients, I give them the same drug; it’s not rocket science that it’s going to work for some but not others, and some may see side effects and others may not.
“This is the biggest trial to show treatment improves with an individualized approach — and I think research into personal cancer vaccines is going to increase dramatically after this positive study.”
Getting to know you — and your disease
Though vaccines are typically associated with disease prevention, in this instance the mRNA vaccine is used to treat people who have already been diagnosed with melanoma.
Samples of tissue are taken and analyzed to identify neoantigens, proteins that form on cancer cells, and which are unique to an individual’s tumor.
Up to 34 neoantigens may be identified, which are then added to an mRNA molecule and added to a vaccine.
The result is a personalized cancer treatment, with the neoantigens most likely to develop an immune response to help the patient’s body fight cancer.
Professor Khattak said it appeared to be more effective after an extended period of time and required multiple doses.
“In this study, the survival rate between the two groups is the same after 40 weeks, so early relapses happen for both,” he said.
“Some patients have fairly resistant tumors that aren’t going to respond to either of the treatments.
“But after the first 40 weeks, by then the patients have had two or three vaccine doses and the anti-tumor effect really kicks in.
“We see quite a significant proportion of patients relapsing after they finish pembrolizumab, whereas we’re not seeing such late relapses in patients who have done the double treatment because in addition to pembrolizumab, the effect of the vaccine kicks in with a much stronger anti-tumor immune response.”
Next steps
Professor Khattak will soon lead a new global trial of the treatment,
His clinic in Perth, Western Australia recruited the most participants of any site in the world.
“I would like to thank all my patients who took part in this research at a difficult point in their life,” Professor Khattak said.
The new trial will include more participants, some with earlier stages of melanoma.
“Stage two and stage three patients combined constitute quite a significant proportion of patients who could be potentially cured, rather than waiting for them to develop metastatic or advanced disease where most of them will not be curable,” he said.
If successful, the trial could be the starting point of a new approach to cancer treatment, beyond just melanoma.
“This is going to be the stepping stone for a number of trials,” Professor Khattak said.
“Because now they have expanded it into lung cancer, kidney cancers, and also into gastrointestinal cancers.
“This has the potential of becoming a new standard of care moving forward.”
Meeting: 2023 American Society of Oncology
Those looking for details on the trial can contact One Clinical Research.
The research was funded by Moderna, Merck Sharp and Dohme.







Be the first to comment on "Revolutionizing Cancer Treatment: The Power of Personalized Vaccines"