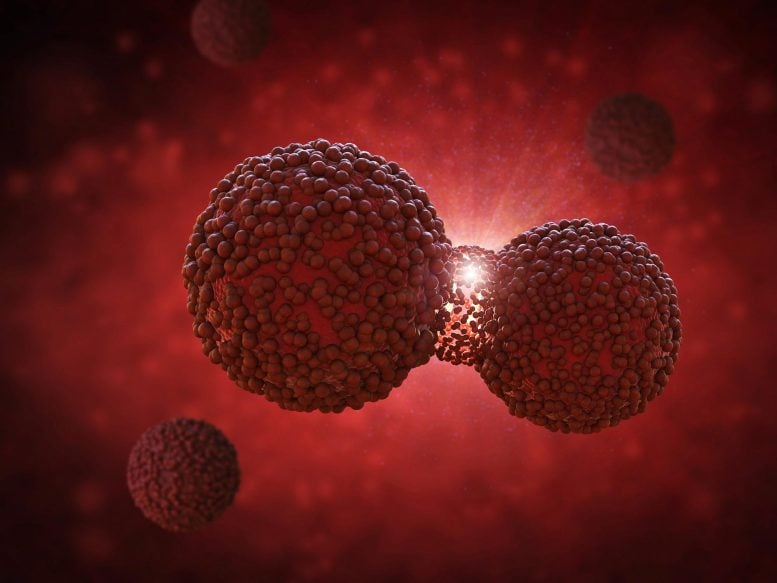
Researchers in the U.S. have compared the cancer risk from agricultural pesticide use to that of smoking, discovering that in some cases, pesticide exposure’s impact on cancer rates is as significant as smoking. The study highlights that a combination of various pesticides, rather than a single type, poses significant health risks, akin to a “cocktail” of chemicals contributing to increased cancer incidences.
Researchers evaluated the effects of common agricultural pesticides on cancer rates, discovering that the use of these pesticides is linked to a higher risk of cancer.
In contemporary agriculture, pesticides are crucial for maintaining high crop yields and ensuring food security. However, these chemicals can negatively impact plant and animal life, as well as pose risks to human health.
Now, in a population-based, nationwide study, researchers in the US have put increased cancer risk through agricultural pesticide use into context with smoking, a better-understood cancer risk factor. The results were published in Frontiers in Cancer Control and Society.
“In our study, we found that for some cancers, the effect of agricultural pesticide usage is comparable in magnitude to the effect of smoking,” said the study’s senior author, Dr Isain Zapata, associate professor at the Rocky Vista University, College of Osteopathic Medicine in Colorado.
Contextualizing cancer risk
“We accept that a person who is not a farmer living in a community with heavy agricultural production is exposed to many of the pesticides used in their vicinity. It becomes part of their environment,” Zapata said.
The researchers found that in such an environment, the impact of pesticide use on cancer incidence rivaled that of smoking. The strongest association was among non-Hodgkins lymphoma, leukemia, and bladder cancer. In these types of cancers, the effects of pesticide exposure were more pronounced than the effects of smoking.
“We present a list of major pesticide contributors for some specific cancers, but we highlight strongly that it is the combination of all of them and not just a single one that matters,” Zapata pointed out.
Pesticide cocktails
Because pesticides aren’t used one at a time, the researchers said it is unlikely that one alone is to blame. Although some pesticides are discussed more frequently than others, all – and mostly their combination – can have an impact. Accordingly, the researchers included 69 pesticides for which use data is available via the United States Geological Survey. “In the real world, it is not likely that people are exposed to a single pesticide, but more to a cocktail of pesticides within their region,” Zapata said.
The researchers said their study is the first comprehensive evaluation of cancer risk from a population-based perspective at a national level. So far, no large-scale study has examined the big picture and put pesticide use in context with a cancer risk factor that is no longer questioned, in this case, smoking. “It is difficult to explain the magnitude of an issue without presenting any context, so we incorporated smoking data. We were surprised to see estimates in similar ranges,” Zapata said.
Seeing the bigger picture
The researchers said that while their study extends knowledge about pesticide use in the US, cancer risk factors are complicated, and assessing the big picture may not reflect individual outcomes. For example, geography has a strong impact. In regions where more crops are grown, such as the Midwest, which is famous for its corn production, the associations between pesticides and cancer incidence were more striking.
Getting people, also those who are not exposed to pesticides frequently, to think about the problems pesticide use poses in a bigger context is one of the researchers’ goals.
“Every time I go to the supermarket to buy food, I think of a farmer who was part of making that product. These people often put themselves at risk for my convenience and that plays a role in my appreciation for that product. It definitely has had an impact on how I feel when that forgotten tomato in the fridge goes bad and I have to put it in the trash,” said Zapata.
Reference: “Comprehensive assessment of pesticide use patterns and increased cancer risk” by Jacob Gerken, Gear Thomas Vincent, Demi Zapata, Ileana G. Barron and Isain Zapata, 5 June 2024, Frontiers in Cancer Control and Society.
DOI: 10.3389/fcacs.2024.1368086







I am a medical anthropologist cancer researcher. One cultural factor that impacts the effect of pesticides on the human body is the use of clothing, especially tight clothing. When these toxins enter the body through the lungs, skin, or intestines, they course throughout the body and into the tissues. The body must eliminate these toxins, usually using the liver and kidneys. But the toxins must first be flushed out of the tissues. This requires the lymphatic system, which consists of microscopic vessels that drain fluid, and the toxins therein, from the tissue spaces to the lymph nodes and ultimately back to the bloodstream. However, these lymphatic vessels are easily constricted and compressed by tight clothing, including belts, underwear, socks, and bras. This results in reduced ability to eliminate these cancer-causing toxins, exposing the tissues to these poisons for longer periods of time relative to no tight clothing. This is why there is a link between wearing tight bras and breast cancer. Unfortunately, the cancer industry does not consider the impact of tight clothing on the body, so they ignore this vital variable. See my article Medicine’s Clothing Problem. https://www.academia.edu/121560525/Medicines_Clothing_Problem