
The researchers found that those who had mild cognitive impairment or Alzheimer’s were less active during the morning and afternoon.
A study investigates whether alterations in daily activities might predict the development of Alzheimer’s disease and other forms of cognitive impairment in older people.
According to a recent study from the Johns Hopkins Bloomberg School of Public Health, wearable movement-tracking devices may one day be helpful in giving older adults early warnings of cognitive decline.
Nearly 600 participants in a long-running community-based health study of older adults wore ActiGraph activity monitors, which employ an activity-tracking sensor similar to those used in Fitbits and Apple watches. Participants with normal cognition and those who had Alzheimer’s disease or moderate cognitive impairment had significantly different movement patterns, the researchers discovered. These differences included less activity during waking hours and more fragmented activity during afternoons among the mild cognitive impairment/Alzheimer’s participants.
The results were recently published in the Journal of Alzheimer’s Disease.
“We tend to think of physical activity as a potential therapy to slow cognitive decline, but this study reminds us that cognitive decline may in turn slow physical activity—and we might someday be able to monitor and detect such changes for earlier and more efficient testing to delay and maybe prevent cognitive impairment that leads to Alzheimer’s,” says study lead author Amal Wanigatunga, Ph.D., MPH, assistant scientist in the Department of Epidemiology at the Bloomberg School.
The recent development of wearable activity-tracking devices, now used by tens of millions of individuals worldwide, has provided a significant opportunity for health researchers to measure and follow changes in physical mobility. The devices can give automated, objective measurements of daily physical activity, sleep patterns, heart rate, and blood oxygen levels, and they are often Internet-connected, enabling manufacturers to create datasets comprising millions of users. Previously, researchers did not have as simple access to such huge amounts of health-relevant data.
The aim of the new study was to determine if activity-tracker patterns recorded from a cohort of older adults differ meaningfully between the cognitively normal and the cognitively impaired. Alzheimer’s disease, the most common form of dementia, is known to be a decades-long process, and researchers generally expect that future disease-modifying interventions will be more effective when started earlier in the disease course. If scientists could identify a distinctive change in activity that predicts the slide into mild cognitive impairment and, eventually, Alzheimer’s and other forms of dementia, then in principle older individuals who show this change in activity could be given further cognitive testing—and, when available, earlier treatment.
The study made use of data from a larger, ongoing health research project known as the Baltimore Longitudinal Study of Aging (BLSA), in which the National Institute on Aging has been studying thousands of people in the Baltimore area since 1958. The analysis was based on 585 BLSA participants for whom sufficient activity-tracker data and cognitive assessments were available during the period July 2015–December 2019. These included 36 participants with either mild cognitive impairment or Alzheimer’s diagnoses.
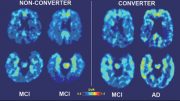
Adjusting for differences based on age, sex, and race, the researchers found that overall differences in all-day activity measures were not strongly different between the mild cognitive impairment/Alzheimer’s and normal cognition groups. However, when the researchers focused on activity patterns during certain times of the day, some differences were revealed.
In the mornings (6 a.m. to noon) and even more so in the afternoons (noon to 6 p.m.), the mild cognitive impairment/Alzheimer’s group had significantly lower measures of activity compared to the normal group. The most striking finding was that activity “fragmentation”—a breaking-up of activity into smaller time periods—was 3.4 percent higher for the mild cognitive impairment/Alzheimer’s participants during the afternoon period.
“Seeing this difference in the afternoons was interesting—one of the main symptoms of Alzheimer’s dementia is the ‘sundowning’ phenomenon involving increased confusion and mood changes that start in the afternoon, and it might be that these activity markers are capturing some movement related to these symptoms,” Wanigatunga says.
The findings, he notes, are preliminary because of the cross-sectional, “snapshot” nature of the study design, though they do support the idea that cognitive decline into mild cognitive impairment and dementia is accompanied by changes in activity patterns.
He and his colleagues plan additional studies that will follow participants over time, to see if measurable yet slight changes in everyday activity patterns help capture early symptomology of mild cognitive impairment and subsequent Alzheimer’s disease dementia.
Reference: “Daily Physical Activity Patterns as a Window on Cognitive Diagnosis in the Baltimore Longitudinal Study of Aging (BLSA)” by Amal Wanigatunga, Fangyu Liu, Hang Wang, Jacek Urbanek, Yang An, Adam Spira, Ryan Dougherty, Qu Tian, Abhay Moghekar, Luigi Ferrucci, Eleanor Simonsick, Susan Resnick and Jennifer Schrack, 19 July 2022, Journal of Alzheimer’s Disease.
DOI: 10.3233/jad-215544
The study was funded by the National Institute on Aging.







Be the first to comment on "Wearable Activity-Trackers Could Provide an Early Warning of Dementia"