
A recent study highlights the detrimental effects on bone strength and bone marrow fat in adolescents and young adults who undergo sleeve gastrectomy, a common weight-loss surgery. The research emphasizes the significance of understanding these implications, especially during the crucial bone-building adolescent years, to ensure proper medical care and monitoring post-surgery.
A study published in Radiology, the journal of the Radiological Society of North America (RSNA), has revealed that a common weight-loss surgery for overweight adolescents and young adults may have adverse impacts on bone health.
“Childhood obesity is on the rise and weight-loss surgery is the most effective way to reduce weight and improve cardiometabolic comorbidities,” said the study’s lead investigator, Miriam A. Bredella, M.D., professor of radiology at Harvard Medical School in Boston, Massachusetts, and vice chair for Faculty Affairs and Clinical Operations, Department of Radiology Massachusetts General Hospital in Boston. “This is the first study in adolescents and young adults that examined the long-term effects of sleeve gastrectomy, the most common type of weight-loss surgery, on bone strength and bone marrow fat.”
Sleeve gastrectomy removes approximately 75% to 80% of the stomach to restrict food intake and induce weight loss. It results in a typically round stomach taking on the shape of a tube or sleeve. The estimated number of sleeve gastrectomy procedures performed each year increased from over 28,000 surgeries in 2011 to over 122,000 in 2020, according to the American Society for Metabolic and Bariatric Surgery. Sleeve gastrectomy has overtaken gastric bypass as the primary weight-loss operation.
For the study, participants between the age of 13 and 24 years were enrolled from 2015 to 2020. The adolescents and young adults had moderate to severe obesity. The young adults had a body max index (BMI) of 35 or above. A BMI of 30 or above is considered obese. Adolescent participants were at 120% of the 95th age- and sex-specific percentile.
There were 54 participants, 25 who underwent sleeve gastrectomy and 29 who were in the control group. Forty-one study participants were female. The surgical group included participants with at least one obesity-related co-morbidity or a BMI at or above 40. The control group had obesity but did not plan to undergo sleeve gastrectomy but received dietary and exercise counseling.
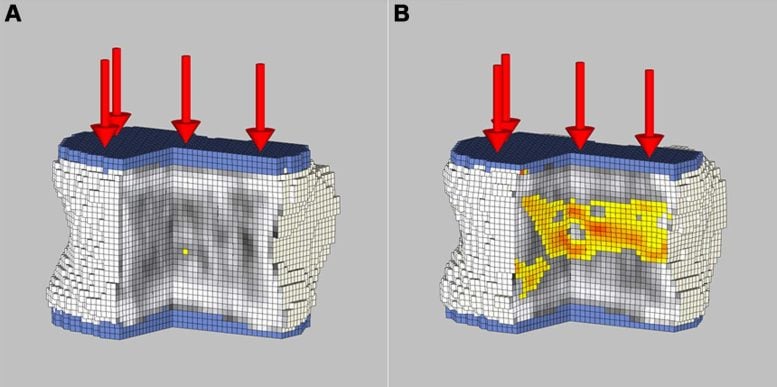
Biomechanical non-contrast CT analysis of the L1 vertebra in an 18-year-old woman with severe obesity (body mass index [BMI], 48.4 kg/m2) prior to sleeve gastrectomy (SG) and 24 months after surgery (BMI, 26.6 kg/m2). L1 vertebra was loaded to 9820 N at both visits for comparison purposes. Breaking strength was (A) 11 920 N at baseline prior to SG and (B) 9820 N at 24 months after surgery. Cutout views of the finite element models under compressive load depict the distribution of bone mineral density (black and white areas) and bone failure (colored areas). Red indicates tissue that failed earlier during the compressive load (weaker bone). Shades of gray indicate different bone densities, with white being dense bone and black being little or no bone mineral. Credit: Radiological Society of North America
Studies have shown that bone marrow fat responds to changes in nutrition and may serve as a biomarker for bone quality. Therefore, patients underwent proton MR spectroscopy to quantify bone marrow fat of the lumbar spine.
Two years following surgery, BMI in the adolescents and young adults dropped (-11.9, on average), while there was a slight rise in BMI in the control group (+1.5, on average). Compared to the controls, sleeve gastrectomy patients had a significant increase in bone marrow fat and a decrease in bone density and strength estimates in the lumbar spine.
“We found that bone strength was lower two years after weight-loss surgery, while bone marrow fat, a marker of bone weakening, was increased, suggesting that weight-loss surgery has negative effects on bone health,” Dr. Bredella said.
Dr. Bredella points out that the adolescent years are a critical time for building up bone mass, and deficits in bone accrual during these years could have a long-term impact on bone health and fracture risk in this younger population later in life.
“As bariatric surgery is increasingly performed in adolescents, its effect on bone health needs to be emphasized, especially to the physicians who will continue to provide routine medical care for these patients,” Dr. Bredella said. “We hope that our study will raise awareness on the effects of weight-loss surgery on bones in adolescents with obesity.”
Raising awareness of the importance of bone health will allow for monitoring and management of low bone mass, optimal dietary supplementation with vitamin D and calcium, and the initiation of appropriate therapy, if necessary, Dr. Bredella noted.
“Our observed effects of weight-loss surgery on bone strength and bone marrow fat might also identify new targets for novel therapies,” she said.
Reference: “Two-year Skeletal Effects of Sleeve Gastrectomy in Adolescents with Obesity Assessed with Quantitative CT and MR Spectroscopy” by Florian A. Huber, Vibha Singhal, Shubhangi Tuli, Imen Becetti, Ana Paola López López, Mary L. Bouxsein, Madhusmita Misra and Miriam A. Bredella, 13 June 2023, Radiology.
DOI: 10.1148/radiol.223256








Put. Down. The. Spoon.