
Researchers at Buck Institute have identified the role of insoluble proteins in aging and Alzheimer’s disease, uncovering their widespread presence beyond just amyloid and tau proteins. Their study in worms demonstrates that boosting mitochondrial health can reverse the detrimental effects of these protein aggregates, suggesting new treatment strategies for neurodegenerative diseases and aging by targeting mitochondrial health and overall protein insolubility.
Researchers at Buck have uncovered connections and proposed interventions aimed at addressing the vicious cycle of protein clumping in Alzheimer’s disease and normal aging.
Insoluble protein aggregates accumulating in the brain are a recognized characteristic of Alzheimer’s disease and other neurodegenerative disorders. Similarly, during normal disease-free aging, there is an accumulation of these insoluble proteins.
To date, approaches to treatments for Alzheimer’s disease have not addressed the contribution of protein insolubility as a general phenomenon, instead focusing on one or two insoluble proteins. Buck researchers have recently completed a systematic study in worms that paints an intricate picture of the connections between insoluble proteins in neurodegenerative diseases and aging. Furthermore, the work demonstrated an intervention that could reverse the toxic effects of the aggregates by boosting mitochondrial health.
“Based on our discoveries, targeting insoluble proteins could provide a strategy for the prevention and treatment of a variety of age-related diseases,” said Edward Anderton, PhD, a postdoctoral fellow in Gordon Lithgow’s lab and co-first author of a study that appears in the May 16 issue of the journal GeroScience.
“Our study shows how maintaining healthy mitochondria can combat protein clumping linked to both aging and Alzheimer’s,” said Manish Chamoli, PhD, a research scientist in Gordon Lithgow’s and Julie Andersen’s lab, and co-first author of the study. “By boosting mitochondrial health, we can potentially slow down or reverse these harmful effects, offering new ways to treat both aging and age-related diseases.”
Results Support the Geroscience Hypothesis
The strong link between insoluble proteins promoting normal aging and diseases also builds a case for the bigger picture of how aging and age-related diseases occur. “We would argue that this work really supports the geroscience hypothesis that there is a common pathway to Alzheimer’s disease and aging itself,” said Buck Professor Gordon Lithgow, PhD, Vice President of Academic Affairs, and the senior author of the study. “Aging is driving the disease, but the factors that put you on the track toward the disease actually occur very early.”
The fact that the team found a core insoluble proteome enriched with numerous proteins that had not been considered before creates new targets for exploration, said Lithgow. “In some ways, it raises the flag about whether we should be thinking about what Alzheimer’s looks like in very young people,” he said.
Beyond Amyloid and Tau
The focus of most research on Alzheimer’s disease to date has been targeting accumulations of two proteins: amyloid beta and tau. But there are actually thousands of other proteins in these insoluble aggregations, said Anderton, and their role in Alzheimer’s disease was unknown. Additionally, he added, their lab and others have observed that during the normal disease-free aging process there is also an accumulation of insoluble proteins. These insoluble proteins from aged animals, when mixed with amyloid beta in the test tube, accelerate the aggregation of the amyloid.
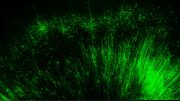
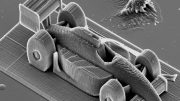
What was the connection between the accumulation aggregates of Alzheimer’s and disease-free aging, the team wondered. Focusing on the amyloid beta protein, they used a strain of the microscopic worm Caenorhabditis elegans, long been used in aging studies, that has been engineered to produce human amyloid protein.
Anderton said the team suspected they might see that amyloid beta is driving some level of insolubility in other proteins. “What we found is that amyloid beta causes a massive amount of insolubility, even in a very young animal,” said Anderton. They found that there is a subset of proteins that seem to be very vulnerable to becoming insoluble, either by adding amyloid beta or during the normal aging process. They called that vulnerable subset the “core insoluble proteome”.
The team went on to demonstrate that the core insoluble proteome is full of proteins that have already been linked to different neurodegenerative diseases in addition to Alzheimer’s disease, including Parkinson’s disease, Huntington’s disease, and prion disease.
“Our paper shows that amyloid could be acting as a driver of this normal aging aggregation,” said Anderton. “Now we’ve got clear evidence, I think for the first time, that both amyloid and aging are affecting the same proteins in a similar way. It’s quite possibly a vicious cycle where aging is driving insolubility and amyloid beta is also driving insolubility, and they’re just making each other worse.”
The amyloid protein is very toxic to the worms and the team wanted to find a way to reverse that toxicity. “Since hundreds of mitochondrial proteins become insoluble both during aging and after expressing amyloid beta, we thought if we can boost the mitochondrial protein quality using a compound, then maybe we can reverse some of the negative effects of amyloid beta,” said Anderton. That’s exactly what they found, using Urolithin A, a natural gut metabolite produced when we eat raspberries, walnuts, and pomegranates which is known to improve mitochondrial function: it significantly delayed the toxic effects of amyloid beta.
“Something that was glaringly obvious from our dataset is that the importance of mitochondria keeps coming up,” said Anderton. A takeaway, the authors say, is the reminder that the health of mitochondria is critical to overall health. “Mitochondria have a strong link with aging. They’ve got a strong link with amyloid beta,” he said. “I think ours is one of the few studies that shows that insolubility and aggregation of those proteins might be the link between the two.”
“Because the mitochondria are so central to all of this, one way to break the vicious cycle of decline is to replace damaged mitochondria with new mitochondria,” said Lithgow. “And how do you do that? You exercise and follow a healthy diet.”
Reference: “Amyloid β accelerates age-related proteome-wide protein insolubility” by Edward Anderton, Manish Chamoli, Dipa Bhaumik, Christina D. King, Xueshu Xie, Anna Foulger, Julie K. Andersen, Birgit Schilling and Gordon J. Lithgow, 16 May 2024, GeroScience.
DOI: 10.1007/s11357-024-01169-1
The study was funded by the National Institute on Aging and the Larry L. Hillblom Foundation.






As only a senior lay American male I am not at all qualified to comment on the use of “Urolithin A” to improve mitochondrial function and cognition. But, on my own, I have arrived at a similar conclusion as it applies to mitochondria. As early as 2019 I wrote Dale Bredesen at the Buck Institute of some of my early lay findings pertaining to multiple chronic illnesses. The following is my most recent update:
“Approximate etiology and pathology of most chronic disease (T = uncertain time): nearly subclinical non-IgE-mediated allergy reactions + offending foods + T + MSG/soy (minimally; less T) > inflammation + T > xanthine oxidase + T > serum uric acid (gout) + ROS (free radicals) + T > immunodeficiency + T > calcium (minimally) loss + T > acidic blood + T > mitochondria switching from glycolysis (glucose-to-energy) to glycogenesis (glucose-to-fat) + T > uric acid deactivating nitric oxide + T > oxidative stress + T > insulin resistance + T > metabolic syndrome (chronic fatigue, aches, pains, muscle weakness and brain fog) + T > chronic/degenerative disease (aging, Alzheimer’s, ALS, AMD, anxiety, bad moods [confusion; depression; mass shootings; suicides], cancer, cataracts, CFS/ME & FM, diabetes, gout, HBP, insomnia, obesity, PD, stroke, tinnitus, tooth loss, etc.) and/or medical error + T > premature disability and/or death.”
While effective treatments for existing victims of Alzheimer’s disease would be a good thing, I believe prevention based on individual allergy awareness and the banning some toxic food additives would be vastly superior.
thank you