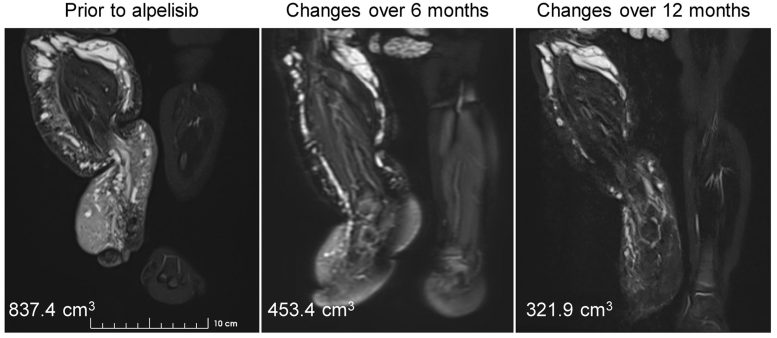
MRI shows the reduction in vascular malformations and leg size induced by alpelisib treatment. Credit: © 2022 Morin et al. Originally published in Journal of Experimental Medicine. https://doi.org/10.1084/jem.20212148
PIK3CA-related overgrowth spectrum (PROS) is a group of rare, incurable disorders caused by mutations in the PIK3CA gene that result in the malformation and overgrowth of various parts of the body. A new report to be published today (January 26, 2022) in the Journal of Experimental Medicine (JEM) describes the successful treatment of two young infants with PROS using the breast cancer drug alpelisib.
PROS encompasses a group of diseases that, taken together, is thought to affect around 1 in 70,000 people. Mutations in the PIK3CA gene alter the growth and proliferation of cells, causing the malformation or excessive growth of various tissues, including the brain, blood vessels, muscle, and bone, which often results in severe disability and premature death.
Though some PROS symptoms can be alleviated through surgery and other forms of palliative care, there are currently no medical treatments approved to treat the disease. However, alpelisib, a PIK3CA inhibitor recently approved to treat certain forms of breast cancer, has shown promising results in both animal models of PROS and a small number of adult and older pediatric patients. The drug is now being investigated in a series of larger clinical trials, but, until now, there have been no data on alpelisib’s efficacy in young infants with PROS.
In the new JEM study, a team of researchers led by Professor Guillaume Canaud (Necker-Enfants Malades Hospital, AP-HP; Université Paris Descartes; Inserm) identified two young patients—an 8-month-old girl and a 9-month-old boy—with a variety of severe symptoms caused by mutations in the PIK3CA gene. These symptoms included extreme blood vessel malformations and asymmetrical overgrowth of limbs and digits, as well as, in the boy’s case, an enlarged right brain hemisphere associated with epileptic spasms.
Daily oral doses of 25 mg alpelisib induced a rapid and significant clinical improvement in all of these symptoms. In the girl’s case, for example, 12 months of alpelisib treatment reduced the amount of vascular malformations and substantially decreased the size of her right leg, allowing her to stand and walk with assistance, while the boy’s epileptic spasms were greatly reduced.
The children’s overall development appeared to be significantly improved, and neither patient showed any adverse effects of alpelisib treatment. Further analyses revealed that, at a daily dose of 25 mg, the levels of alpelisib that accumulated in the children’s blood were much lower than the levels that can be safely tolerated by adults.
“Given the well-established safety profile of alpelisib at the approved 300-mg dose in adults, these low exposures support the continuous treatment of 25 mg alpelisib in these young patients with PROS,” Canaud says. “The results of alpelisib treatment in these two infants are encouraging, but they should be interpreted with caution and will have to be confirmed by future studies.”
Reference: “Treatment of two infants with PIK3CA-related overgrowth spectrum by alpelisib” by Gabriel Morin, Caroline Degrugillier-Chopinet, Marie Vincent, Antoine Fraissenon, Hélène Aubert, Célia Chapelle, Clément Hoguin, François Dubos, Benoit Catteau, Florence Petit, Aurélie Mezel, Olivia Domanski, Guillaume Herbreteau, Marie Alesandrini, Nathalie Boddaert, Nathalie Boutry, Christine Broissand, Tianxiang Kevin Han, Fabrice Branle, Sabine Sarnacki, Thomas Blanc, Laurent Guibaud and Guillaume Canaud, 26 January 2022, Journal of Experimental Medicine.
DOI: 10.1084/jem.20212148








Be the first to comment on "Cancer Drug Shows Promise in Treating Infants With Incurable Disease That Causes Tissue Overgrowth"