Thomas Jefferson University researchers discovered that the SARS-CoV-2 virus could increase the risk of brain cell death found in Parkinson’s disease.
According to a recent study, the coronavirus can increase the mouse brain’s susceptibility to a toxin that causes the death of nerve cells seen in Parkinson’s disease
COVID-19 patients commonly report symptoms such as brain fog, headaches, and insomnia. These neurological complications after a viral infection are not new; in fact, it took patients nearly a decade to develop the neurological disease known as “post-encephalic parkinsonism” after the 1918 influenza pandemic. In a recent study with mice, Jefferson and colleagues demonstrate that the SARS-CoV-2 virus that caused the COVID-19 pandemic could raise the likelihood of the brain degeneration found in Parkinson’s disease.
“Parkinson’s is a rare disease that affects 2% of the population above 55 years, so the increase in risk is not necessarily a cause for panic,” says Richard Smeyne, Ph.D., Director of the Jefferson Comprehensive Parkinson’s Disease and Movement Disorder Center at the Vickie and Jack Farber Institute for Neuroscience and first author of the study. “But understanding how coronavirus impacts the brain can help us prepare for the long-term consequences of this pandemic.”
The study, published on May 17 in the journal Movement Disorders, expands on prior findings from the Smeyne lab indicating that viruses can increase the susceptibility of brain cells or neurons to damage or death. In that earlier study, the researchers discovered that mice exposed to the H1N1 influenza strain that caused the 2009 flu pandemic were more vulnerable to MPTP, a toxin known to cause some of the characteristic symptoms of Parkinson’s disease, most notably the loss of neurons that express the chemical dopamine and increased inflammation in the basal ganglia, a brain region that is crucial for movement. Researchers in Denmark verified the results in people, showing that influenza more than quadrupled the probability of acquiring Parkinson’s disease within 10 years of initial infection.
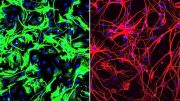
The new study employed mice that were genetically altered to express the human ACE-2 receptor, which the SARS-CoV-2 virus utilizes to get access to the cells in our airways. These mice were infected with SARS-CoV-2 and then allowed to recover. Importantly, the dosage used in this research corresponds to a mild COVID-19 infection in people, with around 80% of infected mice surviving. Thirty-eight days after the surviving mice had recovered, one group was given a modest dosage of MPTP that would not ordinarily trigger neuron loss. The control group was given saline. The animals were sacrificed and their brains were examined two weeks later.
The researchers discovered that COVID-19 infection alone had no impact on dopaminergic neurons in the basal ganglia. However, mice given a modest dosage of MPTP after recovering from infection demonstrated the classic pattern of neuron loss found in Parkinson’s disease. This increased sensitivity following COVID-19 infection was comparable to what was reported in the influenza trial, suggesting that both viruses might cause an equal increase in the risk of developing Parkinson’s.
“We think about a ‘multi-hit’ hypothesis for Parkinson’s – the virus itself does not kill the neurons, but it does make them more susceptible to a ‘second hit’, such as a toxin or bacteria or even an underlying genetic mutation,” explains Dr. Smeyne.
Both influenza and SARS-CoV2 have been found to cause a “cytokine storm” or an overproduction of pro-inflammatory chemicals. These chemicals can cross the blood-brain barrier and activate the brain’s immune cells – microglia. Indeed, the researchers found increased numbers of activated microglia in the basal ganglia of mice that recovered from SARS-CoV2 and received MPTP. While the mechanism is not fully understood, the researchers believe the increased microglia inflame the basal ganglia and cause cellular stress. This then lowers the neurons’ threshold to withstand subsequent stress.
This study was co-led by collaborator Peter Schmidt, Ph.D., a neuroscientist from New York University. “We were concerned about the long-term consequences of viral infection,” Dr. Schmidt said. “Dr. Smeyne is a leader in this area of research and Jefferson was the ideal site to perform the analysis.”
The researchers are planning to determine whether vaccines can mitigate the experimental increase in Parkinson’s pathology linked to prior SARS-CoV-2 infection. They are also testing other variants of the virus, as well as doses that correspond to milder cases in humans.
While their findings thus far bolster a possible link between the coronavirus and Parkinson’s disease, Dr. Smeyne says there are some important caveats. “First of all, this is preclinical work. It is too soon to say whether we would see the same thing in humans, given that there seems to be a 5-10 year lag between any changes in clinical manifestation of Parkinson’s in humans.” This lag, he says, however, could be used to our advantage. “If it does turn out that COVID-19 increases the risk of Parkinson’s, it will be a major burden on our society and healthcare system. But we can anticipate that challenge by advancing our knowledge of potential ‘second hits’ and mitigating strategies.”
This work was supported by a grant from the State of North Carolina and NIH R21 NS122280. The authors report no conflict of interest.
Reference: “COVID-19 Infection Enhances Susceptibility to Oxidative Stress-Induced Parkinsonism” by Richard J. Smeyne Ph.D., Jeffrey B. Eells Ph.D., Debotri Chatterjee BA, Matthew Byrne BS, Shaw M. Akula Ph.D., Srinivas Sriramula Ph.D., Dorcas P. O’Rourke DVM and Peter Schmidt Ph.D., 17 May 2022, Movement Disorders.
DOI: 10.1002/mds.29116




Be the first to comment on "Catching COVID-19 Could Increase Your Risk of Parkinson’s Disease"