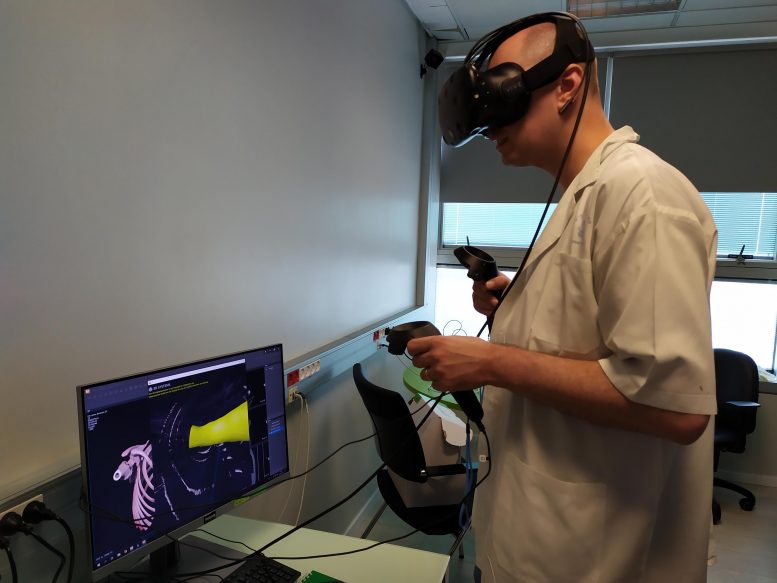
The day before surgery, the treating anesthesiologist spent time on the virtual reality simulator familiarizing himself with the patient’s airway anatomy. Credit: European Society of Anaesthesiology
An anesthesia team in Israel has become one of the first to use 3D printing and virtual reality to produce an exact model of the airway of a 7-year-old girl in order to prepare properly for an operation to remove part of her lung. This pioneering report is published in this month’s edition of the European Journal of Anaesthesiology (the journal of the European Society of Anaesthesiology [ESA]).
The young girl required part of her right lung to be removed due a case of Ewing’s Sarcoma (a bone and soft tissue cancer) spreading to her lung. However, because of her small size (just 18kg or 40lb at the time of the operation), her doctors had concerns that conventional tubing and devices used for lung operations in older patients may not be appropriate and thus decided to use CT scans to create a virtual reality program of her airway/windpipe and lungs, and also an exact 3D printed plastic model so they could practice the operation beforehand.
“Despite the extensive adult experience, our familiarity with one lung ventilation(OLV) in the very young pediatric population is limited,” says Dr. Ruth Shaylor of the Division of Anesthesia, Pain and Intensive Care, Tel Aviv Sourasky Medical Center, Tel Aviv, Israel, the lead author on the report. “We used a combination of 3D printing and virtual reality bronchoscopy to develop a personalized airway plan reducing the potential for trial and error in airway manipulation during the operation.”

Size 5.0-mm endotracheal tube directed down the left main bronchus. Credit: European Society of Anaesthesiology
The day before surgery, the treating anesthesiologist spent time on the virtual reality simulator familiarising himself with the patient’s airway anatomy. Thereafter, the model was used to formulate an individualized airway plan. The 3D model was made of hard plastic, because the team felt that anything more flexible might mean something larger than the patient could tolerate might be used.
The VR and 3D model meant that some of the equipment originally planned for the operation was changed. After the girl was placed under anesthesia, they were able to safely isolate and ventilate her left lung and perform the surgery to remove part of her right lung. “During the procedure, the treating anesthesiologist reported a good correlation between the patient’s anatomy and the VR model, allowing the operation to proceed as planned,” says Dr. Shaylor. “At the end of the procedure, the tubing and equipment were removed easily and the patient made an uneventful recovery.”
“To date, the use of 3D printing in anesthesia has been mainly for educational purposes, she concludes. “3D printing in anesthesia is underutilized for patient-specific pre-operative planning. The same applies to the use of virtual reality in anesthesia. We successfully combined both technologies to produce a personalized airway plan for a child patient. The final airway plan was substantially different to the plan developed using standard imaging techniques. This reduced the number of attempts at lung isolation that would have otherwise been performed on the patient.”
Reference: “The use of three-dimensional printing and virtual reality to develop a personalised airway plan in a 7.5-year-old child” by Ruth Shaylor, Vladimir Verenkin, Eran Golden and Idit Matot, European Journal of Anaesthesiology.
DOI: 10.1097/EJA.0000000000001184









Be the first to comment on "Doctors 3D Print Exact Model of 7-Year-Old Girl’s Airway to Prepare for Delicate Operation"