
In early New England pandemic days, emergency visits dropped by a third, raising concerns about patients avoiding care due to COVID-19 fears.
Despite a surge in COVID-19 cases, emergency department visits declined by nearly a third in five Boston-area hospitals during the early days of the pandemic.
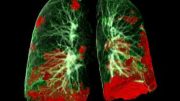
During the early days of the COVID-19 pandemic in New England, emergency department visits for medical emergencies — including psychiatric problems, trauma, and heart attacks — declined by nearly a third, raising concerns among clinicians that critically ill patients were not seeking the care they needed for fear of coronavirus infection.
Comparing emergency department (ED) visits in two major urban hospitals and three community hospitals in the Mass General Brigham system for the months of March and April 2020 with the same period in 2019, Joshua J. Baugh, MD, MPP, Sayon Dutta, MD, MPH, and colleagues in the Department of Emergency Medicine at Massachusetts General Hospital (MGH) found that ED volumes — the total number of patients treated — declined by 30.9% from one year to the next.
“Our health system experienced decreases in nearly all non-COVID-19 conditions presenting to EDs during the initial phase of the pandemic, including those requiring specialty consultation and urgent inpatient procedures. Findings have implications for both public health and health system planning,” Baugh and colleagues wrote in a study in the American Journal of Emergency Medicine.
“While more people with less serious conditions may have stayed away from the emergency department, many cases that we would not have expected to decrease went down as well,” Baugh says. “For example, people requiring catheterization of their hearts for potential heart emergencies, people requiring appendectomies for appendicitis, people requiring consultation for an acute psychiatric episode — across the board we saw that patients with other conditions weren’t coming in at the rate that they usually do.”
As was widely reported at the time, some patients who might otherwise have sought care for non-emergency conditions opted not to go to a hospital out of fear of contracting COVID-19 during the first surge of the pandemic, and some may have sought care at primary care practices or urgent care clinics.
“Some of the changes we saw may have been attributable to reductions in risk from lockdowns, people driving less, and being outside less, but we don’t think that lifestyle changes adequately account for the full effect that we saw,” says Baugh.
“Obviously, we saw many more patients with COVID-19 who otherwise wouldn’t have been there,” Dutta adds, “and a lot of the resources that those patients needed were available because those other patients did not show up. So this expectation that COVID-19 would add to the overall hospital volume or emergency department volume didn’t turn out to be true.”
The retrospective study included data on all ED patients at five hospitals in the Mass General Brigham health system (formerly Partners HealthCare). The hospitals included MGH and Brigham and Women’s Hospital, both Harvard-affiliated quaternary-care referral hospitals with designated centers of excellence for emergency care of patients with trauma, heart attacks, and strokes. The three other hospitals are community-based centers that included one that is a designated level-three trauma center, heart attack center, and stroke center, and two others that are designated stroke centers.
The investigators drew on electronic health records for data on patient demographics, Emergency Severity Index, primary diagnosis in the ED, bedside procedures performed, subspecialty consultations requested, and related procedures occurring during each patient’s hospital stay.
Reference: “The cases not seen: Patterns of emergency department visits and procedures in the era of COVID-19” by Joshua J. Baugh, MD, MPP; Benjamin A. White, MD; Dustin McEvoy; Brian J. Yun, MD, MBA, MPH; David F.M. Brown, MD; Ali S. Raja, MD, MBA, MPH and Sayon Dutta, MD, MPH, 5 November 2020, American Journal of Emergency Medicine.
DOI: 10.1016/j.ajem.2020.10.081
Other co-authors are Benjamin A. White, MD, Brian J. Yun, MD, MBA, MPH, David F.M. Brown, MD, and Ali S. Raja, MD, MBA, MPH, all from MGH and Harvard Medical School; and Dustin McEvoy from Mass General Brigham Clinical Informatics.








Why not go to the hospital? Corona policies have made it confusing, a hassle, and raised questions about whether or not patients will be welcome there or even allowed. And yes, some people also might be concerned about catching Corona. If allowed to go to the ER or doctor, are you allowed to go through this door or that door? What must you do before going? What if you accidentally encounter Corona and get stuck quarantine? etc. The solution is letting people know they are welcome to come to the doctor or ER and how simple it is!
I had this experience. Went to the ER for severe abdominal pain and they took me straight back to triage then right to a room. Saw the doctor in no time, had labs drawn and a CT scan for what ended up being kidney stones. Got a nice dose of iv pain meds and was released in around 2 or so hours. There was almost no one in the waiting room. I had expected a packed ER but that was not case. Yay for me I got quick care, but I worry about people deferring medical care out of fear.
In May 2020, I went to a covid testing facility for 1 or 3 symptoms only i.e. severe sore throat and slightly elevated temperature about 98 degree F and diarrhea. I called my insurance prior to entering the building at my appointment to find out if this facility is in network or not. I was told by my insurance that there should be NO cost at all to do the COVID test. I ended up receiving the bill from the testing facility for me to pay out of pocket. My diagnosis was NOT covid but something else. How can I get this fix? Any help from my State regulator or consumer protection bureau? I have not paid my bill yet waiting for an answer to pay or not. Please help. Thank you.
I have worked ERs and I knew going in that 50% of the patients were not suitable for ER care. They were lonely, could not afford to buy aspirin and cold meds but the hospital would provide for them and so on. It really came home to me when I broke an ankle on an Easter Sunday and showed up at the hospital ER where I worked. It held 91 beds. There was ONE other patient in the entire ER. She had twisted her ankle helping kids search for Easter Eggs at her local church. The two of us had terrific care by dedicated (and totally bored) staff and we made it out in record time. Yes, it continues today. Nearly 50% of ER patients are on welfare (especially Medicaid and Aid to Dependent Children) and the hospital will feed the kids they bring with them, assign a social worker if they are there because the power is off at home and so on and so on. ERs are the heart and soul of the inner city. You would be surprised at the things we see and do for the people who live on the outside of “polite society” just as we get to the gravely ill cases we take care of when they arrive. All in a day’s work.