
Researchers in Sweden have developed a 3D-printed eye implant to treat diabetes by encapsulating insulin-producing cells. Tested successfully in mice, this technology leverages the eye’s transparency for monitoring and promises advances in cell-based treatments.
Researchers in Sweden have developed a microscale device for implantation in the eye, which presents new opportunities for cell-based treatment of diabetes and other diseases.
Collaboration and Design
Aiming towards encapsulating insulin-producing pancreatic cells and electronic sensors, the 3D-printed device was developed by a team from KTH Royal Institute of Technology and Karolinska Institutet. The researchers reported the results of the work in the journal Advanced Materials.
The collaboration between KTH and Karolinska Institutet enables micro-organs—namely pancreatic islets or islets of Langerhans—to be positioned precisely in the eye without the need for sutures. It offers the possibility of cell-based therapy, for example, to treat Type 1 or Type 2 diabetes, using the eye as a base.

“The eye is our only window into the body, and it’s immune-privileged,” says Anna Herland, senior lecturer in the Division of Bionanotechnology at SciLifeLab at KTH Royal Institute of Technology, and the AIMES research center at KTH and Karolinska Institute. Credit: David Callahan/KTH Royal Institute of Technology
Advantages of the Eye
Anna Herland, senior lecturer in the Division of Bionanotechnology at SciLifeLab at KTH and the AIMES research center at KTH and Karolinska Institutet, says that the eye is ideal for this technology because it has no immune cells that react unfavorably in the first stage of implantation. Its transparency allows visual and microscopic study of what happens to the implant over time.
“The eye is our only window into the body, and it’s immune-privileged,” Herland says.

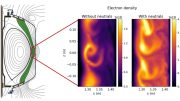
Illustration of the microdevice, and photograph of its position in the eye of a lab mouse. Credit: Hanie Kavand, Montse Visa, Martin Köhler, Wouter van der Wijngaart, Per-Olof Berggren, Anna Herland
Device Design and Functionality
The device is designed as a wedge, about 240 micrometers long, allowing the structure to be mechanically fixed at the angle between the iris and the cornea in the anterior chamber of the eye (ACE). The work demonstrates the first mechanical fixation of a device in the anterior chamber of the eye.
“We designed the medical device to hold living mini-organs in a micro-cage and introduced the use of a flap door technique to avoid the need for additional fixation,” says Wouter van der Wijngaart, professor in the Division of Micro- and Nanosystems at KTH.
Promising Results in Animal Testing
In tests on mice, the device maintained its position in the living organism for several months, and the mini-organs quickly integrated with the host animal’s blood vessels and functioned normally, Herland says.
Per-Olof Berggren, professor of experimental endocrinology at Karolinska Institutet contributed to the research with years of experience in transplanting islets of Langerhans to the anterior chamber of the eye in mice.
“The current unit is unique and will among other things form the basis for our continued work to develop an integrated microsystem for studying the function and survival of the islets of Langerhans in the anterior chamber of the eye,” Berggren says. “This is also of great translational importance, as transplantation of Langerhans islands to the anterior chamber of the eye in humans is subject to clinical trials in patients with diabetes.”
Overcoming Obstacles
Herland says the technology overcomes one obstacle to the development of cell therapies, including those for diabetes. Namely, there is no need for invasive methods to monitor the graft’s function and to guide care in order to ensure long-term transplant success.
“Ours is a first step towards advanced medical microdevices that can both localize and monitor the function of cell grafts,” she says.
She says the design makes it possible to position mini-organs such as organoids and islets of Langerhans without limiting the supply of nutrients to the cells.
“Our design will enable future integration and use of more advanced device functions such as integrated electronics or drug release.”
Reference: “3D-Printed Biohybrid Microstructures Enable Transplantation and Vascularization of Microtissues in the Anterior Chamber of the Eye” by Hanie Kavand, Montse Visa, Martin Köhler, Wouter van der Wijngaart, Per-Olof Berggren and Anna Herland, 10 October 2023, Advanced Materials.
DOI: 10.1002/adma.202306686
The research has been funded by SSF, Knut and Alice Wallenberg Foundation, ERC, Erling Persson Family Foundation and Jochnick Foundation, AIMES and Novo Nordisk Foundation.
The study’s conflict of interest statement notes that Per-Olof Berggren is a partner in Biocrine AB, which is also part of the study.






Try in Rabbits. Try in Goats and Cows. Birds are not mammals, yes. But, their embryos do grow outside mother’s body. I wonder why always mouse and rats? They hatch at the same period as mice?