
A study to be presented at the RSNA meeting shows that higher levels of visceral abdominal fat in midlife are linked to an increased risk of developing Alzheimer’s disease. The research, involving brain scans of 54 participants, indicates that this fat type is associated with early brain changes and inflammation, underscoring its potential as a target for early Alzheimer’s intervention.
Higher amounts of visceral abdominal fat in midlife are linked to the development of Alzheimer’s disease, according to research being presented next week at the annual meeting of the Radiological Society of North America (RSNA). Visceral fat is fat surrounding the internal organs deep in the belly. Researchers found that this hidden abdominal fat is related to changes in the brain up to 15 years before the earliest memory loss symptoms of Alzheimer’s disease occur.
Rising Prevalence of Alzheimer’s
According to the Alzheimer’s Association, there are more than 6 million Americans living with Alzheimer’s disease. By 2050, this number is projected to rise to nearly 13 million. One in every five women and one out of 10 men will develop Alzheimer’s disease in their lifetime.
Identifying Early Alzheimer’s Risks
To try and identify Alzheimer’s risks earlier, researchers assessed the association between brain MRI volumes, as well as amyloid and tau uptake on positron emission tomography (PET) scans, with body mass index (BMI), obesity, insulin resistance and abdominal adipose (fatty) tissue in a cognitively normal midlife population. Amyloid and tau are proteins thought to interfere with the communication between brain cells.
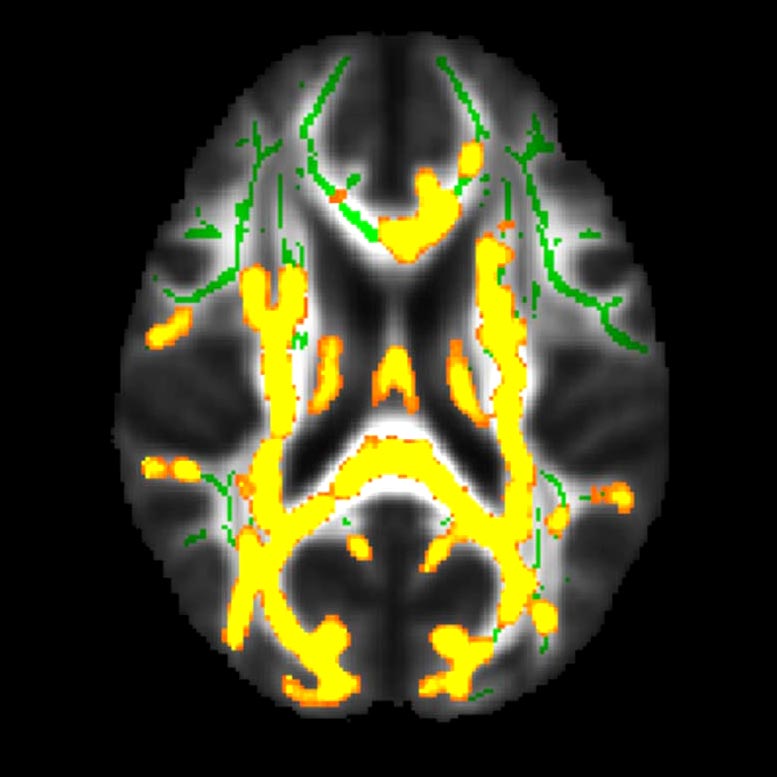
This figure shows increased neuroinflammation (yellow colors) associated with higher hidden fat (visceral fat) in the cohort of 54 participants with an average age of 50 years in the brain’s white matter. The green colors are the normal white matter. Credit: RSNA/Mahsa Dolatshahi, M.D., M.P.H.
Unique Study on Fat Types and Alzheimer’s Risk
“Even though there have been other studies linking BMI with brain atrophy or even a higher dementia risk, no prior study has linked a specific type of fat to the actual Alzheimer’s disease protein in cognitively normal people,” said study author Mahsa Dolatshahi, M.D., M.P.H., post-doctoral research fellow with Mallinckrodt Institute of Radiology (MIR) at Washington University School of Medicine in St. Louis. “Similar studies have not investigated the differential role of visceral and subcutaneous fat, especially in terms of Alzheimer’s amyloid pathology, as early as midlife.”
Study Methodology and Findings
For this cross-sectional study, researchers analyzed data from 54 cognitively healthy participants, ranging in age from 40 to 60 years old, with an average BMI of 32. The participants underwent glucose and insulin measurements, as well as glucose tolerance tests. The volume of subcutaneous fat (fat under the skin) and visceral fat were measured using abdominal MRI. Brain MRI measured the cortical thickness of brain regions that are affected in Alzheimer’s disease. PET was used to examine disease pathology in a subset of 32 participants, focusing on amyloid plaques and tau tangles that accumulate in Alzheimer’s disease.
The researchers found that a higher visceral to subcutaneous fat ratio was associated with higher amyloid PET tracer uptake in the precuneus cortex, the region known to be affected early by amyloid pathology in Alzheimer’s disease. This relationship was worse in men than in women. The researchers also found that higher visceral fat measurements are related to an increased burden of inflammation in the brain.
“Several pathways are suggested to play a role,” Dr. Dolatshahi said. “Inflammatory secretions of visceral fat—as opposed to potentially protective effects of subcutaneous fat—may lead to inflammation in the brain, one of the main mechanisms contributing to Alzheimer’s disease.”
Implications for Early Diagnosis and Intervention
Senior author Cyrus A. Raji, M.D., Ph.D., associate professor of radiology and neurology, and director of neuromagnetic resonance imaging at MIR, noted that the findings have several key implications for earlier diagnosis and intervention.
“This study highlights a key mechanism by which hidden fat can increase the risk of Alzheimer’s disease,” he said. “It shows that such brain changes occur as early as age 50, on average—up to 15 years before the earliest memory loss symptoms of Alzheimer’s occur.”
Dr. Raji added that the results may point to visceral fat as a treatment target to modify risk of future brain inflammation and dementia.
“By moving beyond body mass index in better characterizing the anatomical distribution of body fat on MRI, we now have a uniquely better understanding of why this factor may increase risk for Alzheimer’s disease,” he said.
Additional co-authors are Paul K. Commean, B.E.E., Joseph E. Ippolito, M.D., Ph.D., Tammie L. S. Benzinger, M.D., Ph.D., and John C. Morris, M.D.







Be the first to comment on "Midlife’s Hidden Belly Fat: A Surprising Link to Alzheimer’s Disease"