Prostate cancer is a common type of cancer that affects men, and it occurs in the prostate gland which is a part of the male reproductive system. High-risk prostate cancer refers to aggressive and advanced forms of the disease that are more likely to spread to other parts of the body. The treatment of high-risk prostate cancer can be challenging as it often requires a combination of therapies, including surgery, radiation, and hormone therapy.
According to a phase 2 study conducted by the Johns Hopkins Kimmel Cancer Center and its Bloomberg~Kimmel Institute for Cancer Immunotherapy, the monoclonal antibody enoblituzumab is deemed safe for use in men with aggressive prostate cancer and has the potential to induce clinical activity against cancer throughout the body. If future studies support these findings, enoblituzumab could become the first promising antibody-based immunotherapy agent against prostate cancer.
The clinical trial involved 32 men with high-risk or very high-risk prostate cancer who underwent six weekly infusions of enoblituzumab before their scheduled prostate cancer surgery. The patients were then monitored for an average of 30 months after the procedure. The results were promising, with 66% of the patients, or 21 individuals, exhibiting undetectable levels of prostate-specific antigen (PSA) 12 months post-surgery, indicating the absence of residual disease. The drug was found to be well-tolerated, with no reported surgical delays or medical complications during or after the surgery.
A description of the work was recently publsihed in the journal Nature Medicine.
If enoblituzumab continues to perform well in further larger randomized studies, it could represent a new pathway for immunotherapy against multiple cancers, and the first one that may have a role for prostate cancer, says lead study author and cancer immunology researcher Eugene Shenderov, M.D., Ph.D., assistant professor of oncology at the Johns Hopkins University School of Medicine. Other existing antibody-based immunotherapy drugs have targeted immune checkpoints, natural on/off switches mediating immune responses, such as CTLA-4, PD-1, and LAG-3. Cancer cells hijack these checkpoints, turning off the immune response to cancer. “Drugs that block these checkpoints have had success in other types of cancers, including lung cancer and melanoma, but not in prostate cancer,” says Shenderov.
Enoblituzumab works by binding to a protein called B7-H3 that is overexpressed on prostate cancer cells and believed to impede the immune system’s ability to attack cancer cells. The new therapy could pack a one-two punch against cancer, Shenderov says, by blocking B7-H3’s inhibition of the immune system’s recognition and elimination of cancer cells, and also triggering a process called antibody-dependent cellular cytotoxicity (ADCC), which leads to tumor cell destruction by activating additional immune cells such as macrophages and natural killer cells.
“Enoblituzumab appears safe and seems to activate the immune system in a way that involves both T-cells and myeloid cells,” Shenderov says. “What this means is if these results can be replicated in a larger, randomized study, it opens the possibility that combining this therapy with local, curative-intent therapies like surgical prostate removal or radiation therapy, would allow this drug to potentially kill micrometastatic disease hiding elsewhere in the body, and therefore prevent a significant number of men from experiencing recurring disease. That could be a paradigm shift in prostate cancer.”
The median age of study participants was 64 (age range 48–74). About half (47%) had a PSA greater than 10 ng/mL at diagnosis, which is abnormally high, and 50% had Gleason grade group 5 at biopsy, meaning they had highly aggressive disease. Patients were enrolled from February 2017 through June 2019. Enoblituzumab was confirmed to penetrate into prostate tumors and to bind to B7-H3 in the vast majority of participants, according to prostate samples studied after surgery.
Side effects of enoblituzumab were generally mild and included fatigue, neurological symptoms such as headache or dizziness, and flu-like or cold symptoms. One patient developed inflammation of the heart (myocarditis), which fully resolved with steroid treatment, and is a known side effect of other immune checkpoint drugs.
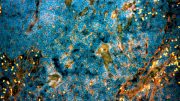
Beyond safety and anti-tumor activity based on PSA dropping to undetectable levels, investigators also looked for changes in the tumor microenvironment before and after enoblituzumab treatment. They found increased markers of cytotoxicity after treatment, consistent with the concept that the immune system was activated against tumor cells. The tumors showed increased infiltration with granulocytes, leukocytes, and effector T-cells, and there was roughly a doubling of the density of cytotoxic T-cells after treatment.
“The findings are exciting but exploratory, and need to be confirmed in larger study cohorts,” cautions senior study author Emmanuel S. Antonarakis, M.D., the Clark Endowed Professor of Medicine and director of GU Oncology for the University of Minnesota Masonic Cancer Center. Antonarakis was the senior investigator of the study while he was at the Johns Hopkins Kimmel Cancer Center.
“However, these results in high-risk prostate cancer patients, and the broader need for immunotherapeutic strategies with efficacy in prostate cancers, provide justification to further develop multipronged approaches that include targeting B7-H3 to optimize antitumor activity in prostate cancers and other solid malignancies,” he says.
Investigators are now planning a larger, randomized trial of enoblituzumab in newly diagnosed prostate cancer patients to assess the clinical activity of the drug compared to current standards of care.
Reference: “Neoadjuvant enoblituzumab in localized prostate cancer: a single-arm, phase 2 trial” by Eugene Shenderov, Angelo M. De Marzo, Tamara L. Lotan, Hao Wang, Sin Chan, Su Jin Lim, Hongkai Ji, Mohamad E. Allaf, Carolyn Chapman, Paul A. Moore, Francine Chen, Kristina Sorg, Andrew M. White, Sarah E. Church, Briana Hudson, Paul A. Fields, Shaohui Hu, Samuel R. Denmeade, Kenneth J. Pienta, Christian P. Pavlovich, Ashley E. Ross, Charles G. Drake, Drew M. Pardoll and Emmanuel S. Antonarakis, 3 April 2023, Nature Medicine.
DOI: 10.1038/s41591-023-02284-w
The study was funded by the National Institutes of Health, NCI SPORE in Prostate Cancer, the Prostate Cancer Foundation Young Investigator Award, the Department of Defense, the Bloomberg~Kimmel Institute for Cancer Immunotherapy, and Macrogenics Inc.
E. Shenderov is a paid consultant to GT Biopharma, Guidepoint Global, FirstThought, GLG, and receives institutional research funding from MacroGenics Inc., manufacturer of enoblituzumab. These relationships are managed by The Johns Hopkins University in accordance with its conflict of interest policies. E. Antonarakis has served as a paid consultant for Janssen, Astellas, Sanofi, Bayer, Bristol Myers Squibb, Amgen, Constellation, Blue Earth, Exact Sciences, Invitae, Curium, Pfizer, Merck, AstraZeneca, Clovis and Eli Lilly; and has received research support from MacroGenics, Janssen, Johnson & Johnson, Sanofi, Bristol Myers Squibb, Pfizer, AstraZeneca, Novartis, Curium, Constellation, Celgene, Merck, Bayer, Clovis and Orion. These relationships are managed by the University of Minnesota (Antonarakis’ current institution) in accordance with their conflict of interest policies.








Be the first to comment on "New Hope for High-Risk Prostate Cancer – Promising Immunotherapy Agent Proven To Be Safe"