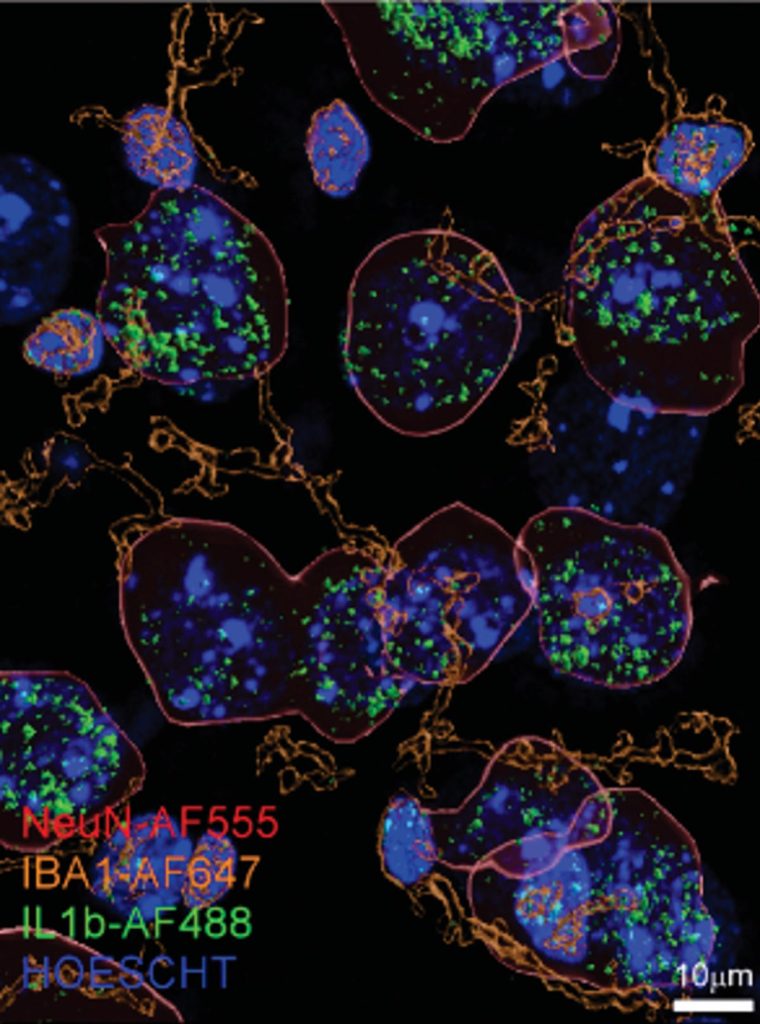
Researchers discovered higher than usual levels of the immune signaling molecule interleukin 1β (green) in neurons (outlined in red) from the brains of alcohol-dependent mice. Credit: Scripps Research
A team of researchers at Scripps has uncovered findings that suggest a new potential target for developing drugs to treat alcohol use disorder.
People with alcohol use disorder (AUD) experience a never-ending vicious cycle of changes in the brain and behavior. AUD can disrupt communication pathways in the brain, leading to an escalation of drinking behavior and further exacerbating the condition.
Scientists at Scripps Research have uncovered new insights into the role of the immune system in the cycle of alcohol use disorder (AUD). In a study published in Brain, Behavior, and Immunity, they found that the levels of the immune signaling molecule interleukin 1β (IL-1β) are elevated in the brains of mice with alcohol dependence. Furthermore, the IL-1β pathway operates differently in these mice, leading to inflammation in crucial regions of the brain that are associated with decision-making.
“These inflammatory changes to the brain could explain some of the risky decision-making and impulsivity we see in people with alcohol use disorder,” says senior author Marisa Roberto, Ph.D., the Schimmel Family Chair of Molecular Medicine and a professor of neuroscience at Scripps Research. “In addition, our findings are incredibly exciting because they suggest a potential way to treat alcohol use disorder with existing anti-inflammatory drugs targeting the IL-1β pathway.”

Alcohol use disorder (AUD) is a medical condition characterized by the inability to control one’s consumption of alcohol, despite experiencing negative consequences such as physical or mental health problems, relationship issues, or problems at work or school. People with AUD may have strong cravings for alcohol, find it difficult to cut back or stop drinking, and may continue to drink despite knowing the harm it can cause. AUD can range from mild to severe and can have a significant impact on a person’s life and well-being. It is important to seek professional help if you suspect that you or someone you know may be struggling with AUD.
AUD is characterized by uncontrolled and compulsive drinking, and it encompasses a range of conditions including alcohol abuse, dependence, and binge drinking. Researchers have previously discovered numerous links between the immune system and AUD—many of them centered around IL-1β. People with certain mutations in the gene that codes for the IL-1β molecule, for instance, are more prone to developing AUD. In addition, autopsies of people who had AUD have found higher levels of IL-1β in the brain.
“We suspected that IL-1β was playing a role in AUD, but the exact mechanisms in the brain have been unclear,” says first author Florence Varodayan, Ph.D., an assistant professor at Binghamton University and former postdoctoral fellow in the Roberto lab.
In the new study, Roberto, Varodayan, and their colleagues compared alcohol-dependent mice with animals drinking moderate or no alcohol at all. They discovered that the alcohol-dependent group had about twice as much IL-1β in the medial prefrontal cortex (mPFC), a part of the brain that plays a role in regulating emotions and behaviors.
The team then went on to show that IL-1β signaling in the alcohol-dependent group was not only increased but also fundamentally different. In mice that had not been exposed to alcohol, as well as in mice that had drunk moderate amounts of alcohol, IL-1β activated an anti-inflammatory signaling pathway. In turn, this lowered levels of the inhibitory neurotransmitter gamma-aminobutyric acid (GABA), a signaling molecule known to regulate neural activity in the brain.
However, in alcohol-dependent mice, IL-1β instead activated pro-inflammatory signaling and boosted levels of GABA, likely contributing to some of the changes in brain activity associated with AUD. Notably, these changes in IL-1β signaling in the alcohol-dependent mice persisted even during alcohol withdrawal.
Drugs that block the activity of IL-1β are already approved by the U.S. Food and Drug Administration to treat rheumatoid arthritis and other inflammatory conditions. More work is needed to determine whether these existing drugs could have utility in treating AUD.
“We plan to follow up on this study with more work on exactly how targeting specific components of the IL-1β pathway might be useful in treating alcohol use disorder,” says Roberto.
Reference: “Chronic ethanol induces a pro-inflammatory switch in interleukin-1β regulation of GABAergic signaling in the medial prefrontal cortex of male mice” by F.P. Varodayan, A.R. Pahng, T.D. Davis, P. Gandhi, M. Bajo, M.Q. Steinman, W.B. Kiosses, Y.A. Blednov, M.D. Burkart, S. Edwards, A.J. Roberts and M. Roberto, 28 February 2023, Brain, Behavior, and Immunity.
DOI: 10.1016/j.bbi.2023.02.020
The study was funded by the National Institutes of Health, The Schimmel Family Chair, The Pearson Center for Alcoholism and Addiction Research, and The Scripps Research Institute’s Animal Models Core Facility.








Be the first to comment on "New Study Reveals How Heavy Alcohol Consumption Increases Brain Inflammation"