
Scientists have developed organoids from stem cells capable of producing dental enamel proteins. The research aims to use these advancements for dental treatments, including repairing damaged teeth or entirely regenerating lost ones.
This advance is viewed as a pivotal initial step toward innovative therapies for the repair and regeneration of teeth.
Stem cells have been used to produce organoids that release the proteins responsible for forming dental enamel, a substance that shields teeth from harm and decay. This initiative was led by a multi-disciplinary team of researchers from the University of Washington in Seattle.
“This is a critical first step to our long-term goal to develop stem cell-based treatments to repair damaged teeth and regenerate those that are lost,” said Hai Zhang, professor of restorative dentistry at the UW School of Dentistry and one of the co–authors of the paper describing the research.
The findings are published today in the journal Developmental Cell. Ammar Alghadeer, a graduate student in Hannele Ruohola-Baker’s laboratory in the Department of Biochemistry at the UW School of Medicine was the lead author on the paper. The lab is affiliated with the UW Medicine Institute for Stem Cell and Regenerative Medicine.
The researchers explained that tooth enamel protects teeth from the mechanical stresses incurred by chewing and helps them resist decay. It is the hardest tissue in the human body.
Enamel is made during tooth formation by specialized cells called ameloblasts. When tooth formation is complete, these cells die off. Consequently, the body has no way to repair or regenerate damaged enamel, and teeth can become prone to fractures or be subject to loss.
To create ameloblasts in the laboratory, the researchers first had to understand the genetic program that drives fetal stem cells to develop into these highly specialized enamel-producing cells.
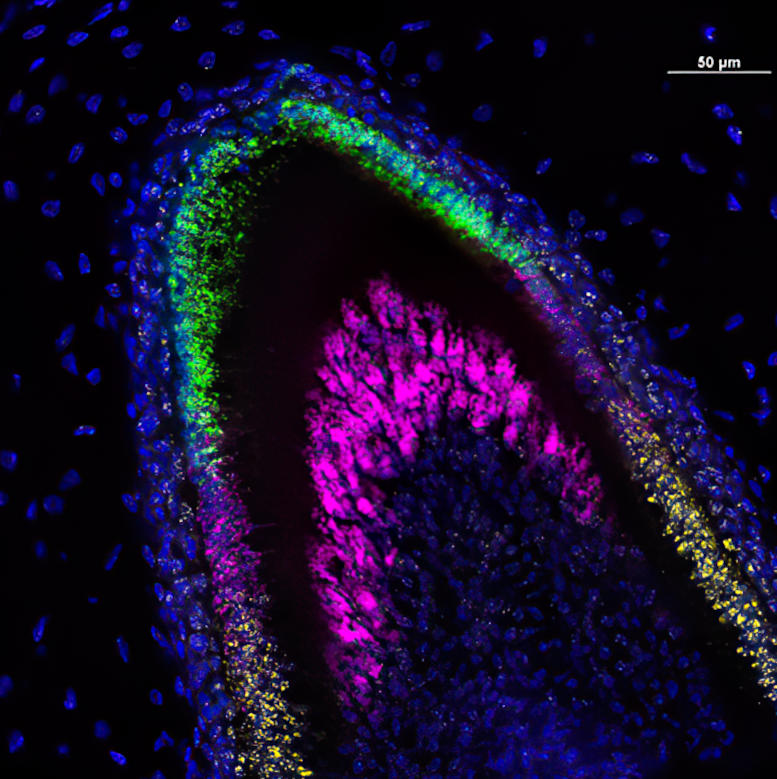
In this lab image of a developing incisor tooth, colors identify which genes are being expressed at each stage of development. Credit: University of Washington Dental Organoid Research Group
To do this they used a technique called single-cell combinatorial indexing RNA sequencing (sci-RNA-seq), which reveals which genes are active at different stages of a cell’s development.
This is possible because RNA molecules, called messenger RNA (mRNA), carry the instructions for proteins encoded in the DNA of activated genes to the molecular machines that assemble proteins. That is why changes in the levels of mRNA at different stages of a cell’s development reveal which genes are turned on and off at each stage.
By performing sci-RNA-seq on cells at different stages of human tooth development, the researchers were able to obtain a series of snapshots of gene activation at each stage. They then used a sophisticated computer program, called Monocle, to construct the likely trajectory of gene activities that occur as undifferentiated stem cells develop into fully differentiated ameloblast.
“The computer program predicts how you get from here to there, the roadmap, the blueprint needed to build ameloblasts,” said Ruohola-Baker, who headed the project. She is a professor of biochemistry and associate director of the UW Medicine Institute for Stem Cell and Regenerative Medicine.
With this trajectory mapped out, the researchers, after much trial and error, were able to coax undifferentiated human stem cells into becoming ameloblasts. They did this by exposing the stem cells to chemical signals that were known to activate different genes in a sequence that mimicked the path revealed by the sci-RNA-seq data. In some cases, they used known chemical signals. In other cases, collaborators from the UW Medicine Institute for Protein Design created computer-designed proteins that had enhanced effects.
Hannele Ruohola-Baker in her stem cell research lab at the University of Washington School of Medicine in Seattle. She recently helped head a study to develop stem-cell-based organoids that could secrete dental enamel proteins. Credit: UW Medicine Institute for Stem Cell and Regenerative Medicine
While conducting this project, the scientists also identified for the first time another cell type, called a subodontoblast, which they believe is a progenitor of odontoblasts, a cell type crucial for tooth formation.
The researchers found that together these cell types could be induced to form small, three-dimensional, multicellular mini-organs, called organoids. These organized themselves into structures similar to those seen in developing human teeth and secreted three essential enamel proteins: ameloblastin, amelogenin, and enamelin. These proteins would then form a matrix. A mineralization process that is essential for forming enamel with the requisite hardness would follow.
Zhang said the research team now hopes to refine the process to make an enamel comparable in durability to that found in natural teeth and develop ways to use this enamel to restore damaged teeth. One approach would be to create enamel in the laboratory that could then be used to fill cavities and other defects.
Ruohola-Baker points out that another more ambitious approach would be to create “living fillings” that could grow into and repair cavities and other defects. Ultimately, the goal would be to create stem cell-derived teeth that could replace lost teeth entirely.
Ruohola-Baker said teeth are an ideal model to work on the development of other stem cell therapies.
“Many of the organs we would like to be able to replace, like human pancreas, kidney, and brain, are large and complex. Regenerating them safely from stem cells will take time,” she said. “Teeth on the other hand are much smaller and less complex. They’re perhaps the low-hanging fruit. It may take a while before we can regenerate them, but we can now see the steps we need to get there.”
She predicts, “This may finally be the ‘Century of Living Fillings’ and human regenerative dentistry in general.”
Reference: “Single-cell census of human tooth development enables generation of human enamel” by Ammar Alghadeer, Sesha Hanson-Drury, Anjali P. Patni, Devon D. Ehnes, Yan Ting Zhao, Zicong Li, Ashish Phal, Thomas Vincent, Yen C. Lim, Diana O’Day, Cailyn H. Spurrell, Aishwarya A. Gogate, Hai Zhang, Arikketh Devi, Yuliang Wang, Lea Starita, Dan Doherty, Ian A. Glass, Jay Shendure, Benjamin S. Freedman and Hannele Ruohola-Baker, 14 August 2023, Developmental Cell.
DOI: 10.1016/j.devcel.2023.07.013
This work was supported by funding from the U.S. National Institutes of Health, the National Heart, Lung, and Blood Institute Progenitor Cell Biology Consortium, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, UW Medicine Institute of Stem Cell and Regenerative Medicine Fellowships and the Dr. Douglass L. Morell Research Fund. Work conducted in the Institute for Stem Cell and Regenerative Medicine’s Genomics Core was supported by a gift from the John H. Tietze Foundation.









I having dentail problem from long time cavities in my teeth always cool and hot in my teeth pls I need ur perfect advice 🙏 pls reaply in detail and mail me ur faithful ness
Hello,
This has already been done several times; Credontis Ag of Switzerland comes to mind. They have patented items that are not only for sale; there are several dentists in the USA using it, to reverse and protect against cavities. Previous news articles from years past, and science journals indicate that regrowing of teeth has been done before; This news article is just a rehash of things i have followed for over a decade. Tides-Glucib was a anti Alzheimer drug that had remarkable progress in regrowing damaged teeth as a side effect. Please research further to find the truth that this news article denies. Oh and Listen to Rich men North of Richmond by Oliver Anthony………..
Would this approach allow enamel to grow where gum decay has caused recession and exposed teeth surfaces?
Unlike the tiny crystals in dentin, the larger size mineral (hydroxylapatite) in fully-formed enamel has a very high crystallographic preferred orientation, reproducing that will be a problem. Randomly oriented crystals might have a seriously different look and resistance to abrasion.
I have crowding teeth since I started growing teeth more than 75 years ago.
Now I have a mouth of pyorreha.
When will this be available throughout the US.