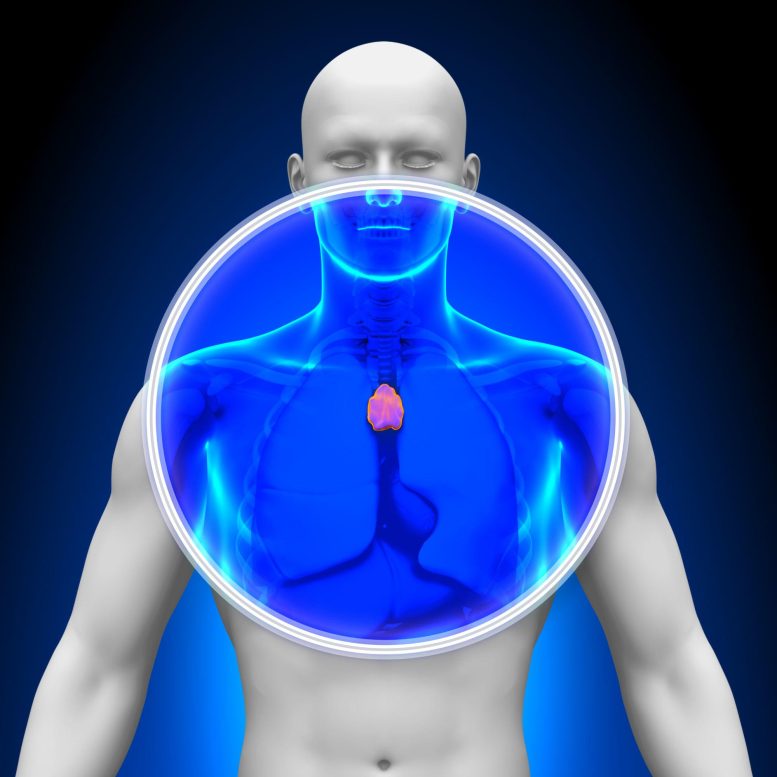
New research led by Harvard has shed light on the critical role the thymus organ plays in maintaining immune health and preventing cancer in adults. The study found that those who had their thymus removed were at a considerably higher risk of death from various causes, including a twofold increase in cancer risk.
Research indicates that a certain organ has a critical role in immune health, especially in the prevention of cancer.
Many people couldn’t say where their thymus is, or what it does, and even doctors have long considered it expendable in adults. However, recent research led by Harvard proposes that this organ, similar in size to a walnut and located in the chest, is essential for maintaining immune health as we grow older, especially in warding off cancer. particularly in cancer prevention.
The research evaluated data from individuals who underwent thymus removal and compared it with those who did not. The findings revealed that the risk of death from various causes, including cancer and autoimmune diseases, was almost three times higher for those who had their thymus removed. Specifically, the risk of cancer doubled, and there was a modest increase in the risk of autoimmune diseases.
“The magnitude of risk was something we would have never expected,” said David Scadden, the Gerald and Darlene Jordan Professor of Medicine and professor in the Department of Stem Cell and Regenerative Biology, who led the study link published in The New England Journal of Medicine in collaboration with researchers at Massachusetts General Hospital.
“The primary reason why the thymus has an impact on overall health seems to be as a way to protect against the development of cancer.”
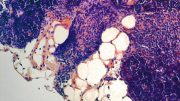
The thymus is the fastest-aging organ, according to Scadden. Most active in churning out T-cells during early childhood, it begins to atrophy into fatty tissue around puberty. That’s why, for many decades, scientists assumed it served a limited purpose in adulthood. It is typically removed due to issues with the organ itself, such as thymus cancer, or during other cardiothoracic surgeries because it’s located in front of the heart and is often in the surgeon’s way.
Yet in recent years scientists had started to suspect that the thymus plays an outsize role in our health as we age, by continuing to make T-cells that contribute to the diversity of the body’s overall T-cell population.
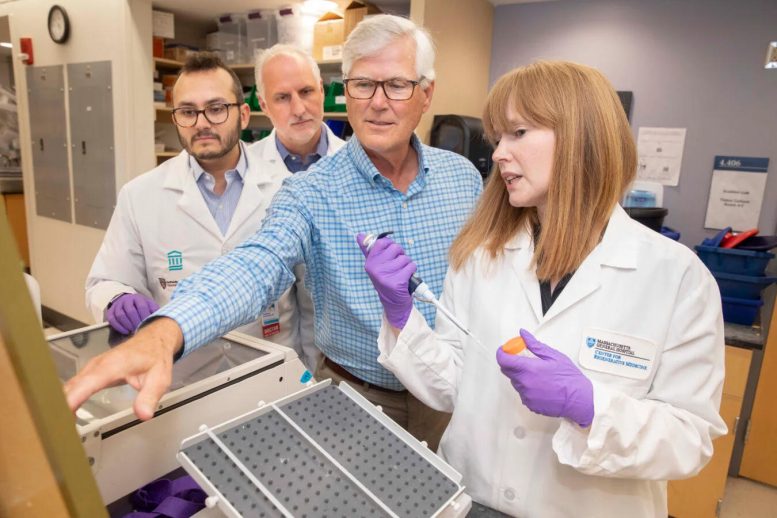
Kameron Kooshesh, (from left), David Sykes, David Scadden, and Karin Gustafsson at work in their lab at MGH. Credit: Kris Snibbe/Harvard Staff Photographer
“This study demonstrates just how vital the thymus is to maintaining adult health,” Scadden said.
First author Kameron Kooshesh became intrigued by open questions about the adult thymus during a second-year neurology lecture at Harvard Medical School. He learned that surgical removal of the thymus is recommended in patients with the autoimmune disease myasthenia gravis as a way to halt T-cell-induced immune destruction of nerve endings. “And yet, clinical instruction on the surgery wards taught me that the thymus is thought to be vestigial in adults,” Kooshesh said. “These two philosophies seemed diametrically opposed, and I yearned to learn more.”
For the study, Kooshesh mined data from 1,146 adult patients who had undergone thymus removal, alongside demographically matched control patients who had undergone similar surgeries but kept their thymus. Kooshesh and Scadden worked in collaboration with Brody Foy, a biostatistician who helped direct the team’s statistical queries around the epidemiology of thymectomy patients, and Karin Gustafsson, an expert in T-cell biology. David Sykes at MGH helped the team facilitate patient blood draws.
In an analysis involving all patients with more than five years of follow-up, the rate of death was higher in the thymectomy group than in the general U.S. population — 9 percent vs. 5.2 percent, as was death due to cancer, or 2.3 percent vs. 1.5 percent.
In a subgroup of patients in whom T-cell production was measured, those who had had their thymus removed had less new production of T-cells, including both helper and cytotoxic T-cells. Those patients also had higher levels of pro-inflammatory cytokines, which are small signaling proteins associated with autoimmunity and cancer, in their blood.
“The magnitude of death and cancer in patients who had undergone thymectomy was the biggest surprise for me,” said Kooshesh, now an internal medicine resident at MGH. “The more we dug, the more we found: The results suggested to us that the lack of a thymus appears to perturb basic aspects of immune function.”
The analysis was facilitated by recent advances in rapid genetic sequencing of T-cell receptors (TCRs). The technology, called TCR sequencing, has enough resolution to allow scientists to not only identify different types of T cells but also measure their diversity as a population overall.
Reference: “Health Consequences of Thymus Removal in Adults” by Kameron A. Kooshesh, Brody H. Foy, David B. Sykes, Karin Gustafsson and David T. Scadden, 3 August 2023, New England Journal of Medicine.
DOI: 10.1056/NEJMoa2302892
The study was funded by the Tracey and Craig A. Huff Harvard Stem Cell Institute Research Support Fund, The Gerald and Darlene Jordan Professorship of Medicine, the National Institutes of Health, the American Society of Hematology, the Swedish Research Council, and the John S. Macdougall Jr. and Olive R. Macdougall Fund.





Next they’ll discover that the tonsils and appendix actually has value in adults and shouldn’t be removed unless absolutely necessary.
Your body is a complete system. All the parts are necessary. Sheese.