
Researchers have conducted a study using gene therapy as a potential treatment for alcohol use disorder (AUD), revealing that sustained release of hGDNF in the brain might prevent relapse into excessive drinking. The study suggests this approach as a promising therapy for AUD, with key findings demonstrating a significant reduction in alcohol intake in treated subjects.
Gene Therapy for Alcohol Use Disorder
Gene therapy might offer a one-time, sustained treatment for patients with serious alcohol addiction, also called alcohol use disorder, according to a new study led by a researcher at The Ohio State University Wexner Medical Center and College of Medicine.
The animal study, published in the journal Nature Medicine, also involved researchers at the Oregon Health and Science University, the Oregon National Primate Research Center and the University of California San Francisco.
Study Details and Findings
The study used an accepted primate model to show that sustained release of glial-derived neurotrophic factor (hGDNF) in a region of the brain called the ventral tegmental area (VTA) may prevent a return to excessive alcohol use after a period of abstinence. Furthermore, it may do so without disrupting other motivated behaviors.
“This gene-therapy approach targets changes in dopamine function in the brain’s mesolimbic reward pathway that are caused by chronic alcohol use,” says co-principal investigator and co-corresponding author Krystof Bankiewicz, MD, PhD, professor of Neurological Surgery and director of the Brain Health and Performance Center at Ohio State. “Our findings suggest that this treatment can prevent relapse without requiring long-term treatment adherence by patients.”
People with alcohol use disorder (AUD) commonly experience repeated cycles of abstinence followed by relapse, even when using one of the few FDA-approved drug therapies, Bankiewicz notes.
Understanding Alcohol Use Disorder
Excessive alcohol use alters certain nerve tracts in the brain that involve the release of the neurotransmitter dopamine. These neurons make up the mesolimbic reward pathway, which plays a major role in alcohol and drug addiction.
These alterations become more pronounced as AUD develops. They include reduced levels of dopamine release, reduced sensitivity of dopamine receptors and increased dopamine uptake. These changes lead to below-normal levels of dopamine in the pathway.
Scientists think this “hypodopaminergic” state can compel excessive alcohol users to resume drinking after periods of abstinence.
“At this time, there are no therapies that target circuits in the brain that are altered by sustained, heavy alcohol use,” says co-principal investigator and co-corresponding author Kathleen Grant, PhD, chief and professor of Behavioral Neuroscience at the Oregon National Primate Research Center.
The Experimental Approach
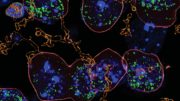
This study used an accepted rhesus macaque model of AUD to examine the practicality and effectiveness of delivering a viral vector into the brain to induce continuous expression of GDNF, diminish alcohol use and prevent post-abstinence resumption of drinking.
Eight male rhesus macaques were involved; the vector was an adenoassociated virus vector that carried a gene for human glial-derived neurotrophic factor (AAV2-hGDNF).
All eight animals were first habituated to the consumption of 4% alcohol. Then four animals were infused with the hGDNF vector directly into the VTA, located in the floor of the midbrain. Neurons in the VTA connect with the mesolimbic reward pathway. The remaining four animals served as controls. They were infused with sterile saline using the same surgical procedure.
Key Findings
- The infusion of AAV2-hGDNF significantly blunted the intake of alcohol across multiple 4-week abstinence and 4-week alcohol-reintroduction cycles;
- Blood ethanol levels were undetectable in GDNF-treated subjects and remained undetectable for most weeks through the study’s end;
- Control subjects showed consistently elevated monthly and weekly alcohol intake and blood ethanol levels across cycles, as a group and individually.
“Overall, our findings indicate that GDNF gene therapy could diminish reintroduction-associated alcohol intake in our primate model,” Bankiewicz says. “We believe this approach shows merit for further study as a promising therapy for AUD and possibly other substance-abuse disorders.”
Alcohol Use Disorder: Statistics and Impact
- An estimated 28.6 million American adults ages 18 and older (11.3% in this age group) and 894,000 adolescents ages 12 to 17 (3.4% of this age group) had AUD in 2021, according to the National Survey on Drug Use and Health.
- An estimated 12% of all alcohol consumers meet the criteria for AUD as defined by the Diagnostic and Statistical Manual for Mental Disorders 5th edition.
- 140,000 deaths per year in the United States are attributed to alcohol use disorder, according to the Centers for Disease Control and Prevention.
For more on this research, see The Power of Gene Therapy in Treating Alcohol Use Disorder.
Reference: “GDNF gene therapy for alcohol use disorder in male non-human primates” by Matthew M. Ford, Brianna E. George, Victor S. Van Laar, Katherine M. Holleran, Jerusha Naidoo, Piotr Hadaczek, Lauren E. Vanderhooft, Emily G. Peck, Monica H. Dawes, Kousaku Ohno, John Bringas, Jodi L. McBride, Lluis Samaranch, John R. Forsayeth, Sara R. Jones, Kathleen A. Grant and Krystof S. Bankiewicz, 14 August 2023, Nature Medicine.
DOI: 10.1038/s41591-023-02463-9
This study was supported by grants from the National Institutes of Health (AA024757, AA013510, AA014091, AA010760, AA019431, OD011092, AA026117).
Other researchers involved in this study were Victor S. Van Laar, Jerusha Naidoo, Piotr Hadaczek, Lluis Samaranch, The Ohio State University; Matthew M. Ford, Lauren E. Vanderhooft, Jodi L. McBride, Oregon National Primate Research Center, Oregon Health & Science University; Brianna George, Katherine M. Holleran, Emily G. Peck, Monica H. Dawes, Sara R. Jones, Wake Forest School of Medicine; Kousaku Ohno, John Bringas, John R. Forsayeth, University of California San Francisco.







Oh-so-many “problem drinkers” are waiting with bated breath to get a drug that makes them able to drink again “like normal drinkers.” AA says: “Many pursure it into the gates of insanity or death.”
Good luck.
“At this time, there are no therapies that target circuits in the brain that are altered by sustained, heavy alcohol use,” This should have said no current Drug therapies. However, many of the theraputic approaches, including meditation and long-term abstinence and self-examination (and CBT) for instance, do have a rather significant impact on the altered circuits in the brain.