
Adverse events were more common in those receiving the drug.
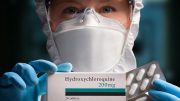
The anti-inflammatory drug hydroxychloroquine does not significantly reduce admission to intensive care or death in patients hospitalized with pneumonia due to COVID-19, finds a study from France published by The BMJ on May 14, 2020.
A randomized clinical trial from China also published on May 14, 2020, shows that hospitalized patients with mild to moderate persistent COVID-19 who received hydroxychloroquine did not clear the virus more quickly than those receiving standard care. Adverse events were higher in those who received hydroxychloroquine.
Taken together, the results do not support routine use of hydroxychloroquine for patients with COVID-19.
Hydroxychloroquine can reduce inflammation, pain, and swelling, and is widely used to treat rheumatic diseases. It is also used as an anti-malarial drug. Lab tests showed promising results, but accumulating trial and observational evidence has called into question whether there are any meaningful clinical benefits for patients with COVID-19.
Despite this, hydroxychloroquine has already been included in Chinese guidelines on how best to manage the disease, and the US Food and Drug Administration (FDA) issued an emergency use authorization to allow the drug to be provided to certain hospitalized patients. The FDA has since warned against use outside clinical trials or hospital settings due to the risk of heart rhythm problems.
In the first study, researchers in France assessed the effectiveness and safety of hydroxychloroquine compared with standard care in adults admitted to hospital with pneumonia due to COVID-19 who needed oxygen.
Of 181 patients, 84 received hydroxychloroquine within 48 hours of admission and 97 did not (control group).
They found no meaningful differences between the groups for transfer to intensive care, death within 7 days, or developing acute respiratory distress syndrome within 10 days.
The researchers say that caution is needed in the interpretation of their results, but that their findings do not support the use of hydroxychloroquine in patients hospitalized with COVID-19 pneumonia.
In the second study, researchers in China assessed the effectiveness and safety of hydroxychloroquine compared with standard care in 150 adults hospitalized with mainly mild or moderate COVID-19.
Patients were randomly split into two groups. Half received hydroxychloroquine in addition to standard care and the others received standard care only (control group).
By day 28, tests revealed similar rates of COVID-19 in the two groups but adverse events were more common in those who received hydroxychloroquine. Symptom alleviation and time to relief of symptoms also did not differ meaningfully between the two groups.
While further work is needed to confirm these results, the authors say that their findings do not support the use of hydroxychloroquine to treat patients with persistent mild to moderate COVID-19.
References:
“Clinical efficacy of hydroxychloroquine in patients with covid-19 pneumonia who require oxygen: observational comparative study using routine care data” by Matthieu Mahévas, Viet-Thi Tran, Mathilde Roumier, Amélie Chabrol, Romain Paule, Constance Guillaud, Elena Fois, Raphael Lepeule, Tali-Anne Szwebel, François-Xavier Lescure, Frédéric Schlemmer, Marie Matignon, Mehdi Khellaf, Etienne Crickx, Benjamin Terrier, Caroline Morbieu, Paul Legendre, Julien Dang, Yoland Schoindre, Jean-Michel Pawlotsky, Marc Michel, Elodie Perrodeau, Nicolas Carlier, Nicolas Roche, Victoire de Lastours, Clément Ourghanlian, Solen Kerneis, Philippe Ménager, Luc Mouthon, Etienne Audureau, Philippe Ravaud, Bertrand Godeau, Sébastien Gallien and Nathalie Costedoat-Chalumeau, 14 May 2020, BMJ.
DOI: 10.1136/bmj.m1844
“Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: open label, randomised controlled trial” by Wei Tang, Zhujun Cao, Mingfeng Han, Zhengyan Wang, Junwen Chen, Wenjin Sun, Yaojie Wu, Wei Xiao, Shengyong Liu, Erzhen Chen, Wei Chen, Xiongbiao Wang, Jiuyong Yang, Jun Lin, Qingxia Zhao, Youqin Yan, Zhibin Xie, Dan Li, Yaofeng Yang, Leshan Liu, Jieming Qu, Guang Ning, Guochao Shi and Qing Xie, 14 May 2020, BMJ.
DOI: 10.1136/bmj.m1849






Thanks for sharing، Keep writing.
Keep in mind this study is not using the other essential elements of the treatment, namely zinc. The hydroxycloroquine only acts as a gateway for the zinc to get into the cells and do the real work. Thus it’s a useless study.
NIH is doing yet another study, without Zinc, which will likely fail. Seems like they are out to prove that Hydroxy does not work.
Our HE MAN in Brazil Mr. Bolosonaro has fired two of his Obstructionist, naysayer health ministers, and has taken charge of the situation. He is going to be starting on DR. Zelenko protocol, hopefully in a few weeks good positive results will emerge. He appears to be more Trumpian, than TRUMP, and he does not have to deal with the lying, lefty media like CNN, MSNBC, …..
Please stop calling observational studies “trials.” Even the title of this article makes it clear this is not a trial.
Trial means that investigators controlled the intervention in an attempt to overcome “indication bias,” where the sickest patients are most likely to get treatment. That was not done in this study and the results are therefore are not definitive. There continues to be no strong evidence for or against hydroxychlorlquine.
A randomized trial is the only real way to determine if any therapy works. There have been no late randomized trials of hydroxychlorlquine. There are several underway. There is little reason to report anything else until these are completed.
This kind of reporting makes it likely that people will just be confused by or ignore the definitive evidence when it is available.
This study and the China study were significantly different then the earlier France study published on the national institute of Health website. This study and the China study used 1200mg daily of hydroxychloroquine only where the earlier France study used 200mg hydroxychloroquine twice daily along with Azithromax. So maybe the takeaway is that less is better. The earlier France study at day 6 post inclusion 100% of patients using hydroxychloroquine and zithromax were virological cured compared to 57.1% with hydroxychloroquine only and 12.5% in the control group. All patients were swabed daily and tested for viral load of Covid 19 during the trial and they found significant viral load reduction each day.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7102549/
This study is bogus. Need to add zinc to the recipe to be effective.