Researchers have found a novel way to combat fungal infections by blocking the fungi’s production of fatty acids. The new compound, NPD6433, has shown effectiveness across a broad spectrum of fungi and offers hope in the face of increasing global drug resistance.
Researchers at the RIKEN Center for Sustainable Research Science (CSRS) and the University of Toronto have discovered an innovative way to combat fungal infections. This method revolves around obstructing the fungi’s ability to produce fatty acids, a primary component of fats. With resistance to anti-fungal drugs increasing, this new tactic, which works differently and is effective against a wide range of fungal species, could prove particularly beneficial. The study was published in the scientific journal Cell Chemical Biology.
The Rising Threat of Fungal Infections
Most people are familiar with athlete’s foot, a relatively benign health issue easily resolved with a trip to the drugstore. However, other fungal infections, caused by Candida, Cryptococcus, and Aspergillus types of fungi, are far more serious. In fact, these fungi are responsible for millions of deaths every year. Like bacteria’s growing resistance to antibiotics, resistance to anti-fungal medications is also on the rise globally. Consequently, the death toll is likely to increase in the foreseeable future without immediate intervention.
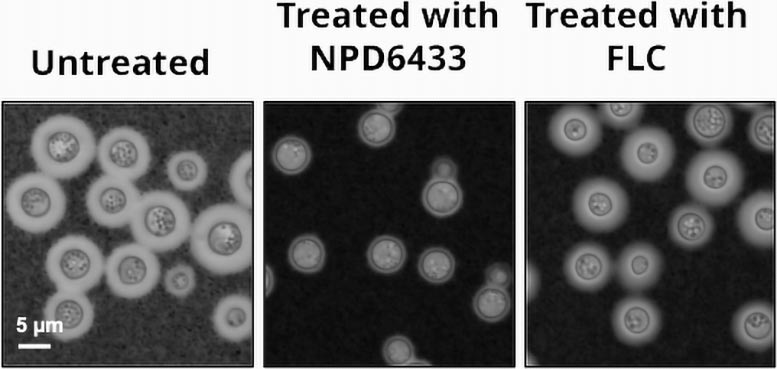
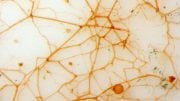
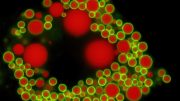
A fungus (C. neoformans) grown in three conditions: untreated, treated with a sub-lethal dose of the fatty acid synthase inhibitor NPD6433, and treated with a fluconazole. The number and virulence of fungi were reduced with NPD6433 treatment. Credit: RIKEN
Presently, only three primary classes of anti-fungal medications exist. All of them function by breaking down the barrier surrounding fungal cells. Interestingly, even though all current treatments target the cell barrier, they are surprisingly species-specific. This specificity implies that a drug effective against one species of fungus might not work on another.
Seeking Broad-Spectrum Anti-Fungal Solutions
The team of researchers sought an alternative strategy to combat harmful fungi, one that could target multiple species. Their approach was to first screen the structurally-diverse RIKEN natural product depository (NPDepo) against four pathogenic yeasts. These include three Candida and one Cryptococcus species, identified by the World Health Organization as critical human pathogens. They aimed to find an agent that would affect all four species, suggesting it could be effective against a broad spectrum of fungi.
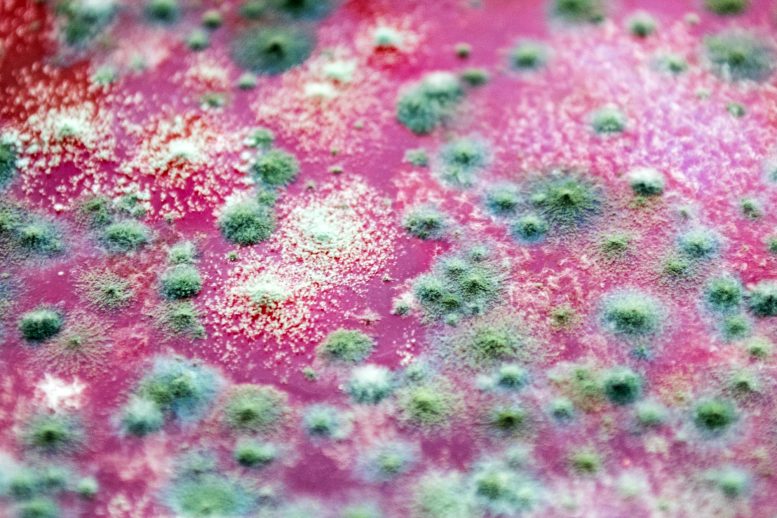
The screening identified several compounds that decreased fungal growth by at least 50% in each of the four species. After eliminating known substances, three new possibilities remained. Among these, the one that was least toxic to human cells also inhibited the growth of Aspergillus fumigatus, a prevalent and deadly fungal mold for immuno-compromised individuals. This compound, named NPD6433 in the RIKEN NPDepo, then underwent further analysis to determine its mechanism of action.
Uncovering the Mechanism of NPD6433
For almost 1000 different genes, the scientists assessed how much NPD6433 suppressed growth in yeast when the yeast was missing one copy of the gene. They discovered that the reduction in only one gene, fatty acid synthase, heightened the yeast’s susceptibility to NPD6433. This indicated that NPD6433 likely functions by inhibiting fatty acid synthase, preventing the synthesis of fatty acids within fungal cells. Subsequent experiments demonstrated that NPD6433 and cerulenin, another fatty acid synthase inhibitor, were capable of exterminating numerous yeast species in culture.
In the final experiment, the researchers tested NPD6433’s efficacy in a live laboratory model organism—the worm Caenorhabditis elegans—which was infected with a pathogenic yeast that can cause systemic infection in humans after invading through the intestines. C. elegans was chosen because it has an intestinal tract that works like ours. Tests showed that treating infected worms with NPD6433 reduced fatalities by about 50%. Importantly, this was true in worms infected with yeast that were resistant to a standard anti-fungal medication.
“Drug-resistant fungi are a growing problem, and leads for the development of new drugs offer hope against these evolving pathogens,” says Yoko Yashiroda, lead RIKEN CSRS author of the study. “Our research indicates that targeting fatty acid synthesis is a promising alternative therapeutic strategy for fungal infections, and one which might not require tailor-made solutions for individual species.”
Reference: “Identification of triazenyl indoles as inhibitors of fungal fatty acid biosynthesis with broad-spectrum activity” by Kali R. Iyer, Sheena C. Li, Nicole M. Revie, Jennifer W. Lou, Dustin Duncan, Sara Fallah, Hiram Sanchez, Iwona Skulska, Mojca Mattiazzi Ušaj, Hamid Safizadeh, Brett Larsen, Cassandra Wong, Ahmed Aman, Taira Kiyota, Mami Yoshimura, Hiromi Kimura, Hiroyuki Hirano, Minoru Yoshida, Hiroyuki Osada, Anne-Claude Gingras, David R. Andes, Rebecca S. Shapiro, Nicole Robbins, Mohammad T. Mazhab-Jafari, Luke Whitesell, Yoko Yashiroda, Charles Boone and Leah E. Cowen, 26 June 2023, Cell Chemical Biology.
DOI: 10.1016/j.chembiol.2023.06.005




Be the first to comment on "Revolutionary Treatment Emerges in the Battle Against Deadly Fungi"