
Recent research indicates that measuring arm fat mass in individuals over 50 could predict their risk of spinal fractures. The study found a negative association between arm fat and spinal bone quality, regardless of BMI. This new metric could lead to more accessible and cost-effective methods for identifying individuals at risk, potentially influencing preventive measures and exercise plans.
Research presented at the 26th European Congress of Endocrinology in Stockholm suggests that measuring the total fat mass in the arms could help predict the risk of spinal fractures in individuals over 50. These findings could lead to simpler and less costly methods for identifying those at high risk and may inform the development of tailored exercise plans.
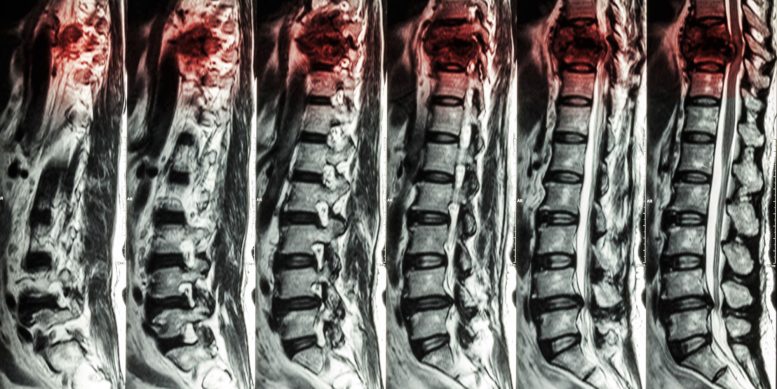
Osteoporosis is a common disease among older people, but is also among the most undiagnosed and untreated medical conditions in the world. Many people do not have noticeable symptoms of osteoporosis until they experience an injury or fracture, which most often occurs in the spine — known as spinal or vertebrae fractures. Imaging techniques, such as dual-energy X-ray absorptiometry (DXA), are used to measure bone mineral density (BMD), while trabecular bone score (TBS) assesses the quality of bone and predicts new fractures independently of BMD. However, the effect body fat has on bone health is still unclear.
New Insights from Recent Research
To investigate this, researchers from the National and Kapodistrian University of Athens in Greece examined 14 men and 101 women, without osteoporosis and with an average age of about 62, and found that those with excess body fat — irrespective of their body mass index (BMI) — had low bone quality (low TBS) in their spine. What’s more, the more belly fat located deep inside the abdomen and around internal organs, the lower the quality of the spine’s spongy bone (or trabecular bone). The researchers then looked at the distribution of body fat under the skin and discovered that individuals with higher fat mass in the arms were more likely to have lower bone quality and strength in the spine.
“Surprisingly, we identified, for the first time, that the body composition of the arms — in particular, the fat mass of the arms — is negatively associated with the bone quality and strength of the vertebrae,” said senior author Professor Eva Kassi.
According to recent research, measuring the total fat mass in the arms could help predict the risk of spinal fractures in people over 50 years old.
“This could mean that the arm’s subcutaneous fat, which can be easily estimated even by the simple and inexpensive skin-fold caliper method, may emerge as a useful index of bone quality of the spine, possibly predicting the vertebrae fracture risk.”
She added: “It should be noted that visceral fat — which we found to be strongly correlated with low bone quality — is the hormonally more active component of the total body fat. It produces molecules called adipocytokines that provoke a low-grade inflammation, so the increased inflammatory status plausibly poses a negative impact on bone quality.”
Professor Kassi acknowledges that larger studies are needed to confirm the link between arm fat and spinal fracture risk. “Although our results remain robust after controlling for age and weight, we will now increase the number of participants and expand the age range by including younger adults between the ages of 30 and 50 years old, as well as more men,” she said.
“Moreover, using the loss of arm fat mass as a marker, we will try to determine the most effective physical exercise routine that not only targets the visceral fat but also focuses on the upper part of the body so that these higher-risk adults lose arm fat and achieve a favorable effect on vertebrae bone quality.”
Meeting: European Congress of Endocrinology









As a now eighty year old lay American male victim, investigator, experimenter and discoverer, I first wrote the US FDA (with replies) of my early lay findings of connections between food allergies (e.g., Arthur F. Coca, by 1935), added MSG (e.g., so-called “Western Diet”), chronic diseases and obesity (obviously, now, in-vain). By early 2009 my allergen avoidance practices, with standard serum testing for calcium being unreliable, made me seriously calcium deficient. In late 2010 I found that high dose liquid calcium capsules with magnesium gluconate tablets and vitamin D3 capsules restored my vitality in about a month. In 2011 I wrote both JACI and The Lancet of my allergy and medical error related calcium deficiency; both declined to publish me. In 2012 and 2015, after years of continuous dosing as described above, ultrasound bone density testing indicated I was still “at moderate risk of osteoporosis.” In mid-March of 2021 I discovered, at-home again, I was very seriously deficient of phosphorus, with calcium carbonate previously known to bind with phosphorus and cause it to be excreted, with my healthcare providers neither warning me nor testing me for phosphorus for nine years. In early 2024 I’m still addressing that with only limited success. On the ‘up’ side, my lumbar vertebra got so soft in 2021 something changed in my low back and I no longer require weekly chiropractic treatments for a partially disabling on-the-job low back injury in 1995. I hope some of this will help researchers to better understand the mostly allergy/uric acid/calcium deficiency connection between visceral fat, soft bones and some joint replacements