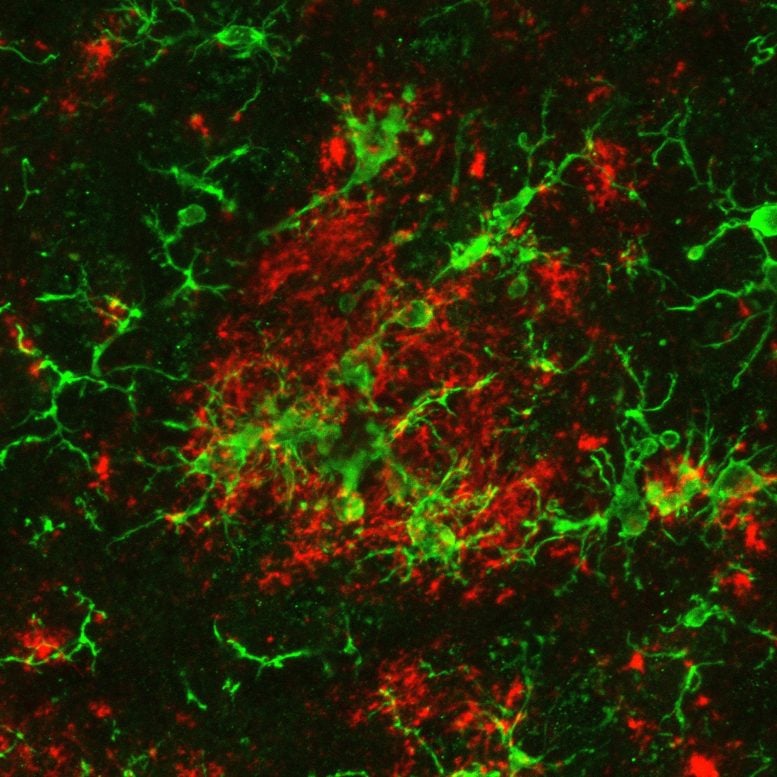
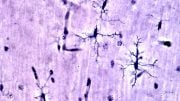
An image of brain immune cells called microglia (green) clustering around a build-up of toxic beta-amyloid (red). Credit: LKCMedicine/NTU Singapore
Researchers have discovered a “metabolic switch” in the brain’s immune cells that could serve as a target for Alzheimer’s disease treatment.
A recent discovery of an “energy switch” within immune cells in the brain holds promise for the creation of drugs to treat Alzheimer’s disease, which is the most widespread form of dementia.
Scientists at Nanyang Technological University in Singapore have uncovered that by blocking and deactivating the aforementioned “switch”, microglial immune cells in the brain were able to remove toxic proteins that can build up and lead to Alzheimer’s disease.
Microglia tend to be damaged in people with the disease, which makes them less capable of clearing cellular toxic waste. To restore the clean-up function, the scientists “switched off” their inefficient metabolism by preventing a key enzyme from attaching to energy-generating parts of the immune cells.
The findings from lab experiments set the stage for developing drugs that can specifically target metabolism in brain immune cells in order to treat Alzheimer’s disease, which contributes to 60 to 70 percent of all dementia cases globally. The World Health Organisation estimates that 78 million people worldwide will have dementia by 2030.
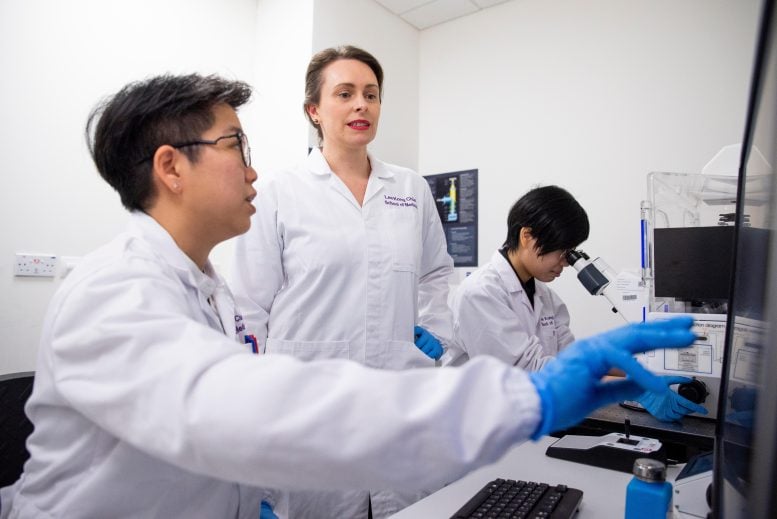
From left: Research fellow Dr Wong Jia Hui, Nanyang Asst Prof Anna Barron, and final year PhD student Ms Lai Kei Onn from Nanyang Technological University, Singapore’s Lee Kong Chian School of Medicine. They are part of the NTU team that discovered a “metabolic switch” in brain immune cells that could be targeted as a potential treatment for Alzheimer’s disease. Credit: NTU Singapore
Such drugs are of high interest in healthcare. While there are ways to treat the symptoms of Alzheimer’s disease, there are currently no definitive cures for the condition, which tends to affect the elderly and impairs people’s ability to think.
The researchers’ findings, which were published in Proceedings of the National Academy of Sciences in February 2023, are in line with one of the goals of the NTU 2025 strategic plan to respond to the needs and challenges of healthy living and aging.
Cracking a metabolism puzzle
The findings of the researchers, led by Nanyang Assistant Professor Anna Barron from NTU’s Lee Kong Chian School of Medicine, stem from their work investigating the function of a biomolecule called the translocator protein, which is found in energy-generating parts of immune cells and which is widely used in clinical research to track inflammation.
Asst Prof Barron’s group had previously shown that drugs that activated this protein led to less toxic waste build-up in the brain, which improved the condition of mice with Alzheimer’s disease. But how this worked was not clear.
The team cracked the puzzle with their latest experiments on cells from mice with Alzheimer’s. Their work revealed that the translocator protein is critical for the microglia immune cells of the brain to generate their own energy.
Microglia perform the important function of “gobbling up” and removing beta-amyloid, a toxic protein whose build-up in the brain causes damage and death to nerve cells, resulting in Alzheimer’s disease. To do their job properly and remove the toxic waste, the immune cells need a lot of energy.
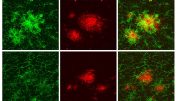
The research team showed that without the translocator protein, microglia from mice with Alzheimer’s had an energy problem and could not remove the beta-amyloid, which resulted in the disease worsening in the mice.
“We found that microglia lacking the translocator protein resembled damaged microglia observed in aging and Alzheimer’s disease,” said Asst Prof Barron. “These damaged microglia inefficiently produced energy and could not clean up toxic waste in mice with Alzheimer’s disease.”
The experiments also demonstrated that when the translocator protein is absent, an enzyme called hexokinase-2, which metabolizes sugar, kicks into action in microglia to compensate. The enzyme promotes an inefficient way for cells to produce energy. What was surprising was that hexokinase-2 became activated when it stuck to the energy-generating parts of cells called mitochondria.
The researchers found that hexokinase-2 was also activated in microglia when exposed to more toxic forms of beta-amyloid, just as happens in Alzheimer’s disease. The scientists believe this finding helps to partly explain how microglia fail in patients with Alzheimer’s disease and when people age.
To manipulate the enzyme’s role in microglia energy production, the NTU researchers developed a light-activated tool. Their tool involves shining blue light onto a genetically modified version of the hexokinase-2 enzyme to “switch off” one of its functions.
When this happens, it blocks the enzyme’s ability to stick to the energy-generating parts of the microglia and forces the cells to stop relying on an inefficient method of energy production. Experimental results showed that this improves their ability to clear beta-amyloid by nearly 20 percent.
However, if hexokinase-2’s sticking ability is not blocked and its function is disrupted by simply inactivating the enzyme, it does not help the microglia to clear away waste. This insight provides a critical clue for future drug targets.
Targeted drug development
Asst Prof Barron said that her team’s findings provide a basis for them to develop drugs that can act specifically on the metabolism of immune cells in the brain to treat Alzheimer’s disease.
For instance, drugs could be developed to prompt the brain’s microglia to produce energy more efficiently and thus clear toxic beta-amyloid proteins to protect against Alzheimer’s disease.
Such drugs could target the hexokinase-2 enzyme, which is found in the brain’s microglia at high levels in people with Alzheimer’s disease.
The team expects targeted drugs for Alzheimer’s disease to be an improvement over those drugs being studied now that do not specifically zero in on metabolism in brain microglia cells.
Dr. Yeo Tianrong, a senior consultant neurologist at Singapore’s National Neuroscience Institute who was not involved in the research, said that Asst Prof Barron and her team were able to gain new insights to piece together the puzzle of energy generation that is needed for microglia to remove beta-amyloid in the brain.
“Importantly, they found that the displacement of hexokinase-2 led to improved energy production and enhanced the microglia’s ability to get rid of beta-amyloid. This is of significance as the strategy of hexokinase-2 displacement represents a potential therapeutic target for improved beta-amyloid removal by the microglia,” said Dr. Yeo.
“The study by Asst Prof Barron’s team highlights the possibility that, one day, we can harness the intrinsic capability of microglia to mop up toxic beta-amyloid by re-configuring their energy generating framework,” he added.
Future research that the team is planning includes experiments in mice to verify that what they observed in cells can be replicated in animals, where physiological conditions may have an unexpected impact on the results.
The approach of controlling metabolism in microglia using the light-activated tool will also prove useful in studying how energy production works in cells for other diseases and conditions, including diabetes and obesity.
“This tool gives us a way to understand how metabolism contributes to diseases. Historically, this has been hard to study because most approaches to control metabolism are irreversible, lead to toxicity, or cannot target cells of interest. However, our tool allows us to control energy processes in specific cells in a reversible way that also doesn’t kill the cells being studied,” said Asst Prof Barron.
Reference: “Mitochondrial control of microglial phagocytosis by the translocator protein and hexokinase 2 in Alzheimer’s disease” by Lauren H. Fairley, Kei Onn Lai, Jia Hui Wong, Wei Jing Chong, Anselm Salvatore Vincent, Giuseppe D’Agostino, Xiaoting Wu, Roshan R. Naik, Anusha Jayaraman, Sarah R. Langley, Christiane Ruedl and Anna M. Barron, 14 February 2023, Proceedings of the National Academy of Sciences.
DOI: 10.1073/pnas.2209177120
The study was funded by the Ministry of Education – Singapore and Nanyang Technological University.





Be the first to comment on "Clearing Toxic Waste Linked to Alzheimer’s – Study Finds Game-Changing Way To Boost Brain Immune Cells"