
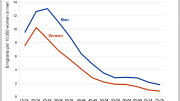
An estimated 25% of older Americans with cognitive decline live alone, leading to various risks and challenges. A recent study indicates that the U.S. health system is ill-prepared to support these individuals, whose needs contrast starkly with better provisions in countries like Europe, Japan, and Canada.
Patients often forget their appointments, confuse their medications, and have no one to contact in an emergency.
Approximately 25% of elderly Americans with dementia or mild cognitive impairment live alone, exposing them to risks such as unsafe driving, wandering, medication confusion, and missed medical appointments.
A study recently published in the journal JAMA Network Open, led by researchers from UC San Francisco, indicated that the U.S. healthcare system is inadequately prepared to cater to the unique needs of individuals living alone with cognitive challenges. This population is expected to grow as the general population ages.
For these patients, living alone is a social determinant of health with an impact as profound as poverty, racism, and low education, said first author Elena Portacolone, PhD, MBA, MPH, of the UCSF Institute for Health and Aging and the Philip R. Lee Institute for Health Policy Studies.
In this qualitative study, researchers interviewed 76 healthcare providers, including physicians, nurses, social workers, case workers, home care aides, and others. Participants worked in memory clinics, home care services, social services, and other places in California, Michigan, and Texas.
The providers raised concerns about patients missing medical appointments, failing to respond to follow-up phone calls from the doctor’s office, and forgetting why appointments were made, leaving them vulnerable to falling off the radar. “We don’t necessarily have the staff to really try to reach out to them,” said a physician in one interview.
Discharging a patient is like ‘sending a kid out to play on the freeway’
Some patients could not assist their doctor with missing information on their chart, leaving the providers uncertain about the pace of their patient’s decline. Many had no names listed as emergency contacts, “not a family member, not even a friend to rely on in case of a crisis,” according to a case manager.
These patients were at risk for untreated medical conditions, self-neglect, malnutrition, and falls, according to the providers. A house service coordinator also noted that calls to Adult Protective Services were sometimes dismissed until a patient’s situation became very serious.
One consequence of the shaky infrastructure supporting these patients was that they were not identified until they were sent to a hospital following a crisis, like a fall or reaction to medication mismanagement. Some were discharged without a support system in place. In one case, a patient was sent home with a taxi voucher, a situation that a psychiatrist likened to “sending a kid out to play on the freeway.”
These findings are an indictment of our health care system, which fails to provide subsidized home care aides for all but the lowest-income patients, said Portacolone.
“In the United States, an estimated 79% of people with cognitive decline have an income that is not low enough to make them eligible for Medicaid subsidized home care aides in long-term care,” she said, adding that the threshold for a person living alone in California is $20,121 per year.
While Medicare is available to adults over 65, subsidized aides are generally only provided after acute episodes, like hospitalizations, for fixed hours and for limited durations, she said.
“Most patients need to pay out-of-pocket and since cognitive impairment can last for decades, it is unsustainable for most people. Aides that are available via Medicaid are very poorly paid and usually receive limited training in caring for older adults with cognitive impairment,” she added.
Subsidized home care aides plentiful in Europe, Japan, Canada
In contrast, subsidized home care aides are generally available to a significantly larger percentage of their counterparts living in parts of Europe, Japan, and Canada, said Portacolone, citing a 2021 review of 13 countries, of which she was the senior author.
The study’s findings illustrate substantial deficiencies in how our health system provides for people with dementia, said senior author Kenneth E. Covinsky, MD, MPH, of the UCSF Division of Geriatrics. “In an era when Medicare is going to spend millions of dollars for newly approved drugs with very marginal benefits, we need to remember that Medicare and other payers refuse to pay far less money to provide necessary supports for vulnerable people with dementia.”
The researchers advocate for a system in which robust supports are made available by funding from an expanded Medicare and Medicaid. This will become increasingly critical, said Portacolone, “because effective treatments to reverse the course of cognitive impairment are unavailable, childlessness and divorce are common, and older adults are projected to live longer and often alone.”
Reference: “Perceptions of the Role of Living Alone in Providing Services to Patients With Cognitive Impairment” by Elena Portacolone, Tung T. Nguyen, Barbara J. Bowers, Julene K. Johnson, Ashwin A. Kotwal, Robyn I. Stone, Sahru Keiser, Thi Tran, Elizabeth Rivera, Paula Martinez, Yulin Yang, Jacqueline M. Torres and Kenneth E. Covinsky, 18 August 2023, JAMA Network Open.
DOI: 10.1001/jamanetworkopen.2023.29913





In addition to that posted earlier today (e.g., https://scitechdaily.com/from-gut-to-brain-new-findings-link-microbiota-to-alzheimers-memory-loss/#comment-816644), I’d like to point it out that in 1787 the Founders prescribed (e.g., Preamble to the US Constitution) America to be a peaceful, prosperous, moderate secular socialist nation-state, not the failed and failing extremist capitalist Christian money, power and war mongering nation-state it is today.
And, two simple solutions to the problem are presently available: 1) ensure everyone has purer, safer diets to delay dementia and serious disability and 2) tax the greedy rich their fair share to pay for what they have caused and are causing, also to better compensate home service providers. My qualifications? After forty-two years and counting of externally imposed chronic illness and partial disability, and having paid up to 33% of my earned income in total annual taxes while working, I’m still living independently at age 79 while more affluent and less well informed seniors are totally dependent and/or dying much younger.